Introduction
Health and Social Care Partnerships (HSCPs) were introduced in 2015 to bring together a range of community health and social care services. The responsibility for organising these services previously lay with Councils and Health Boards, but now sits with HSCP Boards (sometimes called Integration Joint Boards). The idea behind creating HSCPs was to integrate health and social care services much more closely under a single manager, with a single combined budget, delivering a single plan to meet a single set of national outcomes in a way that better meets local needs and removes barriers for people using services. The “single plan” is called the HSCP Strategic Plan. It sets out how HSCP Boards will plan and deliver services for their area over the medium term, using the integrated budgets under their control. In East Dunbartonshire we have integrated a wide range of adult and children’s community health and social care services, including criminal justice services.
All Health and Social Care Partnerships (HSCPs) are required to publish an Annual Performance Review that sets out progress towards the delivery of its Strategic Plan and in pursuance of:
- the nine National Health & Wellbeing Outcomes;
- the development of locality planning and improvement
- financial performance and Best Value
In addition, we have included information on:
- Our performance as assessed through external inspection and regulation
- Good practice examples
Our Priorities
The pressure on delivering health and social care has continued to be intense throughout the period of this report, due in part to the continuing impact and consequences of the Coronavirus pandemic. With fluctuating emergency response arrangements and the impact on services and staffing levels, the HSCP has had to continue to adapt to a fast pace of change and respond quickly to frequently changing circumstances and regulations. This was been particularly felt during the winter months, when pressure on services was exceptional, contributed to by a return to high influenza rates and the rebounding of demand that was inevitably under-presented during successive periods of lockdown. It is clear that it will take a period of time for health and social care capacity to rebalance and recover from the impact of the last three years.
The HSCP and its staff have risen to these challenges and have continued to work to support the most vulnerable people in our community and promote social justice, equality and safety. Our considerable achievements and innovative practice this year are evident in this report. It is also important to note that the pandemic has affected our ability to deliver some of our regular performance targets, due to the impact on services and staff. Where targets have been achieved, it is also important to recognise the external influences that may have impacted on these achievements. For this reason, the review of performance in 2022/23 has to be viewed through the lens of the unique set of circumstances that we have all been living through.
Our focus over the last 12 months has also been to align our priorities to our new HSCP Strategic Plan 2022/25, so this Annual Performance Report will look a little different to previous years, as we have structured it to reflect our new strategic priorities and enablers. Our overall aim continues to be to ensure the people of East Dunbartonshire receive the best service possible in a way that is fair, responsive and person-centred.
We were reminded through our Staff Award nominations this year of the outstanding work delivered on a daily basis by our committed workforce, that so consistently go the extra mile for the people that they support. It felt particularly special to be able to hold the Awards ceremony in person this year, after such a challenging period for everyone.
We would wish to extend our enormous gratitude to all the staff, partners and individuals in the HSCP, to volunteers and community groups, to informal carers and families, for the enormous efforts that they have made to the people we have supported over the last 12 months.
On this page you will find information on:
Strategic Planning and Delivery
How Well Are We Achieving Our Priorities
How Well Are We Developing Our Enablers
Locality Planning
Hosted Services
Other Achievements & Good Practice Highlights
Financial Performance
Inspection & Regulation
Annex 1 - National Outcomes and Local Strategic Priorities & Enablers
Annex 2 - Care Inspectorate Evaluations – Local Services
Annex 3 - Comparative Income & Expenditure 2015/16 – 2022/23
Annex 4 - Achievement of Best Value
Annex 5 - Notes on Performance Data Methodology
Strategic Planning and Delivery
Strategic Plan
Every HSCP Board is required to produce a Strategic Plan that sets out how they intend to achieve, or contribute to achieving, the National Health and Wellbeing Outcomes. Strategic Plans should also have regard to the National Integration Delivery Principles. These national outcomes and principles are set out at Annex 1.
In January 2022, the HSCP Board approved a new HSCP Strategic Plan for the period 2022/25. This new plan reflects on the progress the Partnership has made and sets out the strategic direction for the next three years. Our vision remains unchanged, and our refreshed strategic priorities continue to reflect and support delivery of the national outcomes. Demonstrating our achievement towards these will be the focus of annual performance reporting from this year.
However, it is important to acknowledge that the landscape of health and social care has changed markedly in the few short years since the last plan was published. Our aspiration to improve and develop services and partnerships in our 2018/21 Strategic Plan was affected significantly by financial pressures, which were shared with the Health Board and Council. This was compounded by increasing demand pressures, both in terms of increasing volume and increasing complexity of levels of care. The impact of the Covid-19 pandemic has been substantial and may continue to be felt over the full period of our Strategic Plan 2022/25.
For these reasons, our Strategic Plan 2022/25 has aspirations based on the realities of the pressures being faced in the health and social care sectors and building towards a fair, equitable, sustainable, modern and efficient approach to service delivery. Some of these areas of redesign will take longer than the period of the Strategic Plan to deliver. Without new resource streams, any requirement to invest further in one service area will require greater efficiency or disinvestment in another. Implementing the Plan will also continue to be based on certain assumptions and dependencies that can in reality be fragile. Our overall focus will be to:
- Invest in early intervention and prevention;
- Empower people and communities by encouraging more informal support networks at a local level;
- Ensure that people have access to better information earlier, to allow them to access the right support at the right time, from the right person.
These developments should deliver better outcomes for people and will also make for a more efficient, sustainable system of care and support.
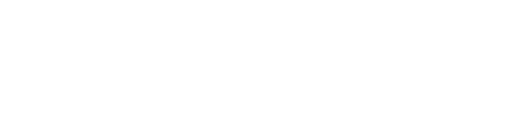
The illustration below provides an overview of the Strategic Plan 2022-25. It shows the relationship between the strategic priorities and enablers and the actions that will be taken forward in support of these.
Annual Delivery Plan
Each year a number of improvement actions in support of the Strategic Plan are drawn down into an Annual Delivery Plan. Supporting detail is held in service-level plans, locality plans and service commissioning plans, which collectively set out how the high level strategic priorities and enablers will be pursued.
The HSCP Board monitors progress in achieving the objectives in the Annual Delivery Plan, regularly throughout the year. The Board achieves this with support from the Strategic Planning Group and the Audit Performance & Risk Committee to ensure active governance over how well these aspects of the Strategic Plan are being implemented.
There were a total of 31 initiatives to be taken forward within the Delivery Plan during 2022/23. Many of these initiatives are expected to take more than one year to complete. By the end of 2022/23, progress towards these projects were as follows:
- 24 were successfully completed.
- 1 was programmed to continue beyond 2022/23, but were on track for completion within their overall timescales.
- 6 were reported to be at risk of delay and will be carried forward into the 2023/24 Delivery Plan or into the Heads of Service Delivery Plan for 2023/24.
A summary of the completed Annual Delivery Plan 2022/23 is set out below, with more detail provided in the priority sections later in the report:
HSCP ANNUAL DELIVERY PLAN 2022/23: PROGRESS
| Initiative | Strategic Plan Priority | Strategic Plan Commitment | National Outcome |
|---|---|---|---|
| Initiatives Successfully Completed By End 2022/23: | |||
| Develop an HSCP Public Health Strategy and refresh objectives for Public Health Improvement Team | Empowering People | Reduce inequality and inequity of outcomes | 1, 2, 3, 4, 5, 6, 7, 9 |
| Redesign of HSCP website | Empowering People | Improving information and communication | 1, 2, 3, 4, 5, 6, 7, 9 |
| Increase uptake of support at a distance | Empowering People | Improve Personalisation | 1, 2, 3, 4, 5, 6, 7, 9 |
| Learning Disability: service review, action plan and implementation | Empowering Communities | Modernising day services | 1, 2, 3, 4, 5, 6, 9 |
| Develop a Social Support for Older People Strategy | Empowering Communities | Modernising day services | 1, 2, 3, 4, 5, 6, 9 |
| Refresh HSCP Locality Plans | Empowering Communities | Building local integrated teams | 1, 2, 3, 4, 5, 6, 9 |
| Identify a staff base in the West locality | Empowering Communities | Building local integrated teams | 1, 2, 3, 4, 5, 6, 9 |
| Review and redefine operational approaches to community-led support | Empowering Communities | Building informal support options | 1, 2, 3, 4, 5, 6, 9 |
| Prioritise Public Protection | Delivering our Key Social Work Public Protection Statutory Duties | Prioritising public protection | 4, 5, 7 |
| Delivery of Year 2 of Children’s House Project | Supporting Families and Carers | Strengthen corporate parenting | 1, 2, 3, 4, 5, 6, 7 |
| Review and update HSCP Carers Strategy | Supporting Families and Carers | Supporting carers with their own needs and in their caring role | 1, 2, 3, 4, 5, 6, 7 |
| Implementation of “The Promise” | Supporting Families and Carers | Implementing The Promise for children and young people | 1, 2, 3, 4, 5, 6, 7 |
| Review current model of Post Diagnostic Support delivery | Improving Mental Health and Recovery | Improve post-diagnostic support for people with dementia | 1, 2, 3, 4, 5, 6, 7 |
| Implement the Children and Young People’s Mental Health and Wellbeing Framework | Improving Mental Health and Recovery | Improve mental health support for children and young people | 1, 2, 3, 4, 5, 6, 7 |
| Review accommodation arrangements in line with Scottish Government guidance and alongside Health Board and Council policies | Post Pandemic Renewal | Understanding and responding to the impact of the pandemic | 1, 4, 5, 8, 9 |
| Develop and implement an organisational development plan in support of staff orientation back to buildings |
Post Pandemic Renewal | Understanding and responding to the impact of the pandemic | 1, 4, 5, 8, 9 |
| Address the backlog in unpaid work services, as alternative to custodial sentences | Post Pandemic Renewal | Understanding and responding to the impact of the pandemic | 1, 4, 5, 8, 9 |
| Review mainstream Covid-19 testing procedures and implement in line with requirements. | Post Pandemic Renewal | Understanding and responding to the impact of the pandemic | 1, 4, 5, 8, 9 |
| Refresh and streamline Personal Protective Equipment (PPE) arrangements | Post Pandemic Renewal | Understanding and responding to the impact of the pandemic | 1, 4, 5, 8, 9 |
| Develop and implement a Joint Commissioning Plan for Unscheduled Care | Maximising Operational Integration | Right Care Right Place: urgent and unscheduled health and social care redesign | 3, 4, 7, 8, 9 |
| Deliver a range of measures to support staff wellbeing | Workforce and Organisational Development | Supporting the wellbeing of the health and social care workforce | 3, 4, 7, 8, 9 |
| Develop an Annual Delivery Plan for 2022/23 | Medium Terms Financial and Strategic Planning | Balancing investment and disinvestment | 1, 2, 3, 4, 5, 6, 7, 8, 9 |
| Review the engagement framework in support of collaborative approaches with third and independent sector providers | Collaborative Commissioning | Co-designing solutions with the third and independent sectors | 1, 2, 3, 4, 5, 6, 7, 8, 9 |
| Develop and implement an HSCP Property Strategy | Infrastructure and Technology | Modernising health and social care facilities | 2, 5, 7, 9 |
| Initiatives with longer term timescales that were on track at end of 2022/23: | |||
| Conclude implementation of the Primary Care Improvement Plan Memorandum of Understanding (2) | Collaborative Commissioning | Supporting Primary Care Improvement | 1, 2, 3, 4, 5, 6, 7, 8, 9 |
| Initiatives with longer term timescales that were delayed at end of 2022/23: | |||
| Develop a compassionate communities model in East Dunbartonshire | Empowering Communities | Building informal support options | 1, 2, 3, 4, 5, 6, 9 |
| Review of Community Occupational Therapy and Reablement services across the HSCP | Prevention and Early Intervention | Extending rehabilitation and re-ablement | 1, 2, 4, 5, 6, 9 |
| Review of commissioned mental health and alcohol and drugs services. Develop action plan for reshaping of services | Improving Mental Health and Recovery | Improving adult mental health and alcohol and drugs recovery | 1, 2, 3, 4, 5, 6, 7 |
| Implement the recommendations from the Public Dental Service review Programme Board | Workforce and Organisational Development | Redesigning the Public Dental Service to support the right care is being delivered in the right place at the right time | 1, 2, 3, 4, 5, 6, 7, 8, 9 |
| Review HSCP organisational structures | Medium Term Financial and Strategic Planning | Maximising available resources | 1, 2, 3, 4, 5, 6, 7, 8, 9 |
| Implement 22/23 Digital Action Plan | Infrastructure and Technology | Maximising the potential of digital solutions | 1, 2, 3, 4, 5, 6, 7, 8, 9 |
PERFORMANCE MANAGEMENT FRAMEWORK
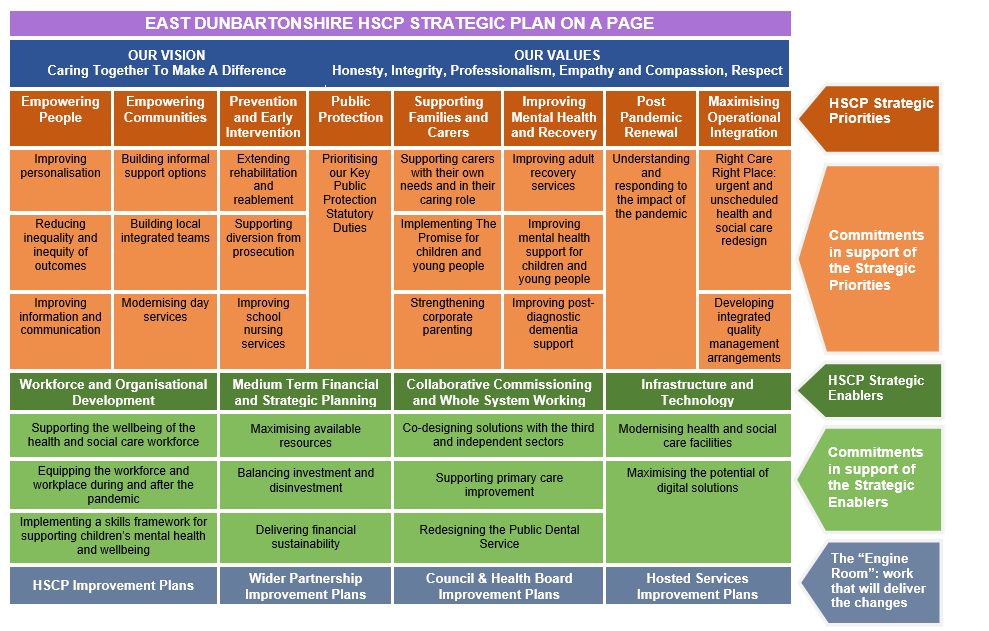
The HSCP has a Performance Management Framework in place that sets out how it measures, monitors and continuously seeks to improve what it does. This is designed to ensure confidence at all levels that it knows how well it is performing, that it knows what should improve and how, and that it knows the impact of any such improvements. The Performance Management Framework also sets out in detail its approach to monitoring and measuring success, including the production of this Annual Performance Report.
The HSCP’s Performance Management Framework provides the overarching statement on how the HSCP ensures scrutiny, self-evaluation and reporting in three main areas:
- The fulfilment of the HSCP Strategic Plan, which is a high level statement of our 3-year strategic priorities and enablers;
- Operational improvement, which should be a continuous process of balancing effectiveness, efficiency and economy, and;
- Quality management, which should involve applying scrutiny and evaluation to ensure that our core services are delivering the best possible experiences and outcomes.
The document sets out the HSCP’s obligations with respect to Best Value, its systematic approach to continuous improvement (including organisational alignment, often called the “golden thread”) and its associated governance arrangements. The diagram at Fig 1 (below) is designed to illustrate the relationships between the Strategic Plan, the Annual Delivery Plan, other subordinate strategies and plans and the reporting of impact and outcomes:
Fig 1: Improvement Planning and Organisational Alignment
A Framework for Community Health and Social Care Integrated Services
In November 2019, the Scottish Government published A Framework for Community Health and Social Care Integrated Services [opens in a new window] which was designed to inform the development of local transformation plans, drawing on what has been found to be effective through impact evaluation. We used this document to support the preparation of our Strategic Plan 2022-25. It inspired the Strategic Plan’s structure that distinguishes strategic priorities from strategic enablers, it provided a checklist for consideration when setting out our programme of action and it provided a foundation of evidence-based approaches to improving service user, informal carer and organisational outcomes. The progress set out in this Annual Performance Report therefore aligns itself strongly with the provisions within the Framework.
How Well Are We Achieving Our Priorities?
This section of the Annual Performance Report sets out our progress and performance towards the achievement of the priorities set out in our HSCP Strategic Plan. It also demonstrates our progress towards the delivery of the National Health and Wellbeing Outcomes, which are cross-referenced at Annex 1.
Under each priority, the report summarises the key highlights and provides more detail on improvements and developments made in each area. A selection of performance information then follows, firstly the national core integration and ministerial indicators (where these apply to the priorities) and then other national and local measures that are used by the HSCP to measure performance. Notes on methodology relating to the performance measures and indicators are set out at Annex 5.
Empowering People
| Our Highlights | |
|---|---|
| Adoption of a range of digital solutions to support self-management. | A refreshed Public Health Strategy developed and approved. |
| New Public Protection website launched, providing more intuitive and accessible information and advice. | Adults with Incapacity Procedures updated and supported with joint training. |
Our Progress
| Objectives for 2022/25 | Progress in 2022/23 |
|---|---|
| Commitment: Improving Personalisation | |
| Embed and further develop digital solutions, to support self-management (Redesign). |
There has been an increase in the technological and digital options available to support self-management and provide support at a distance. These have included:
Work with the Scottish Government to support a local digital maturity assessment to inform our action plan, has not materialised as planned. The HSCP is now looking to participate in a national programme to reflect our readiness and capabilities to take forward the digital agenda. |
| Further develop person centred, rights-based, outcome focused approaches (Improvement). |
In response to the Mental Welfare commission Report “Authority to Discharge” and its recommendations, the HSCP developed and fully implemented an action plan during 2022/23. Our Adults with Incapacity Procedures were reviewed jointly with legal services and updated to reflect additional safeguards and considerations relating to ‘deprivation of liberty’. Leadership sessions and revised training sessions were delivered and rolled out to all relevant HSCP staff. Further work to embed these updated procedures is planned for 2023/24 involving other staff groups including clinical team leads. Social Work has established a Creative and Innovative Directory of Support Packages that describes individualised approaches to meeting people’s personal outcomes that are a bit different from the norm. This Directory is then available for colleagues to generate creative approaches and to share good practice. |
| Commitment: Reducing inequality and inequity of outcomes | |
| Further reduce inequality of health outcomes and embed fairness, equity and consistency in service provision (Improvement). |
A new post of HSCP Communications, Engagement and Equalities Officer has been approved, for deployment during 2023/24. A review of HSCP compliance with the Public Sector Equality Duty was completed during 2023/24 with an action plan in place to advance our position. Based on the National Priorities, a refreshed Public Health Strategy has been draft concluded to facilitate further coproduction and sign-off for implementation. |
| Commitment: Improving information and communication | |
| Improve service information and public communication systems, advice, reflecting specific communication needs and preferences (Improvement). |
In 2022/23, a new Public Protection website was launched, which makes information more accessible and user-friendly. The HSCP’s general website content has been reviewed and updated in preparation for its move to a new platform within its hosted site in East Dunbartonshire Councils website. This should make the information more accessible and intuitive. |
Our Performance
National Integration Indicators Used To Measure This Priority:
This section provides the HSCP’s performance against national core integration indicators (Notes on methodology at Annex 5):
RAG KEY:
 Positive performance improved in 2022/23
Positive performance improved in 2022/23
 Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining performance
Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining performance
 Performance declined in 2022/23
Performance declined in 2022/23
This section provides the HSCP’s performance against Scottish Government Ministerial Strategic Group (MSG) indicators:
Other National and Local Indicators of Performance & Quality:
RAG KEY:
 On target
On target Within agreed variance of target
Within agreed variance of target Below Target
Below Target
| PI Title | 2022/23 | Note | |||
|---|---|---|---|---|---|
| Status | Value | Target | |||
| Empowering People | |||||
| Percentage of people 65+ indicating satisfaction with their social interaction opportunities |  |
95% | 95% | Local performance indicator based on a sample of 50 case reviews analysed each quarter. | |
| Percentage of service users satisfied with their involvement in the design of their care packages |  |
96% | 95% | Local performance indicator based on a sample of 50 case reviews analysed each quarter. | |
| Number of homecare hours per 1,000 population aged 65+ |
|
511 | 389 | Balance of Care. Based on 2022/23 Quarter 4 census period. Aim = to maximise in comparison to support in institutional settings. | |
| Percentage of adults in receipt of social work/social care services who have had their personal outcomes fully or partially met |
|
100% | 100% | As a minimum, outcomes should reduce risks from a substantial to a moderate level, but the arranging of informal support may additionally contribute to improving quality of life. Aim = to maximise. | |
| Smoking quits at 12 weeks post quit in the 40% most deprived areas |  |
19 | 21 | Service facing difficulties due to stock shortages of Varenicline and other Nicotine Replacement Therapies. Data based on 2022 calendar year data. Aim = to maximise. | |
Empowering Communities
| Our Highlights | |
|---|---|
| Opening of the new purpose-built Allander Day Service for adults with learning and intellectual disabilities. | The HSCP Social Support Strategy for Older People 2023-28 was developed and approved. |
| Co-location of services continues, to ensure locally responsive, collaborative and accessible services. | Updated community asset map for people with mental health issues. |
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Objectives for 2022-25 Progress in 2022/23 Commitment: Building informal support options | |
| Work with communities to develop a network of assets and informal supports, to complement formal, statutory support options (Redesign). |
The HSCP has sought to develop and implement a model of community led support locally based on best practice, which seeks to reduce waiting lists and divert needs to alternative effective service options. A series of community drop-in sessions have been piloted to support healthy ageing and independent living. The programme is currently being evaluated to consider development of future delivery options. The HSCP and its partners have also refreshed an Asset Map, which is an interactive tool to support people to find local groups and facilities for their own and others' health and wellbeing. The map is populated by community members and local partners. The HSCP aimed to develop and implement a delivery plan for No One Dies Alone (NODA) within East Dunbartonshire. The start of this project was delayed due to funding issues which was resolved in December 2022, when work commenced. This project will continue to be delivered in 2023/24. The HSCP Older People Local Area Co-ordination team has undertaken excellent work with local people to develop new informal social support groups during 2023/24 (see Part 6). |
| Commitment: Building local integrated teams | |
| Develop local, co-located services with integrated multi-disciplinary teams to improve services and reduce our carbon footprint (Redesign). |
During 2022/23, the co-location of health and social work children and families staff was successfully established, resulting in improved communication, collaboration and relationship building. Locality Planning has now been re-established within the HSCP and will continue to operate though re-established arrangements and supported by the updated locality need and demand profiles. Localities will aim to deliver improved outcomes for local people via collaboration and partnership action and the development and implementation of 2023/24 Locality Plans. The multidisciplinary locality practitioner collaboratives in community health and care services continue to work well to improve outcomes for people and communities. Scope has been identified to expand this model to other care groups. Premises within Milngavie have been identified and suitably adapted for the use of HSCP staff within the West locality, which supports local integrated working. Further work is underway to continue to embed the aspirations of full co-location and integrated working. |
| Commitment: Modernising day services | |
| Redesign day services for older people and adults with learning disabilities, to create a wider range of informal and formal support options (Redesign). |
March 2023 saw the opening of the new purpose-built Allander Day Service for adults with learning and intellectual disabilities. This new space is co-located with the new Allander Leisure Centre, which offers reciprocal access arrangements, progressive activity-based therapies and extensive accessible resources. The new centre is founded on the principles of a community based approach to service delivery. New initiatives have been developed to support employment / employability, community participation and volunteering established to enhance personalised support options and to promote choice, community integration and independence. This year we have established two new Local Area Coordinator posts to support employment initiatives for adults affected by learning disability, learning difficulty and autism. In the first year of operation the team has worked with twenty eight adults of whom fourteen are now in paid employment, fifteen in further education and seventeen within volunteer placements with a number accessing more than one sector. Across all of the HSCP’s day service redesign approaches, there has been a continued focus on developing community-based support alternatives to formal day care with employment opportunities and programmes developed in line with an employability pathway and the continued growth and development of community assets. Following a period of consultation on a new model for the delivery of social support options for older people, the Social Support Strategy for Older People 2023-2028 was developed and approved. The first year of the Strategy involves undertaking activities to commission and develop the agreed day centre model, moving to two rather than three formal centres, and to progress the growth in informal community-based social supports. |
Prevention and Early Intervention
| Our Highlights | |
|---|---|
| Building greater rehabilitation and reablement into care at home services, to promote independence and reduce over-dependence on services | Continuously improving hospital discharge planning arrangements |
| Delivery of Anxiety Management (LIAM) interventions by School Nursing Services. | Extended diversion in Justice Services, to ensure individual needs are met at the earliest opportunity, to enable people to desist from further crime. |
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Extending rehabilitation and reablement | |
| Further develop rehabilitation services and reablement approaches to sustain people for longer in the community (Improvement) |
The HSCP has committed to a review of community Occupational Therapy (OT) and Reablement services, to deliver an improved service model which addresses OT waiting times and maximises use of equipment and digital options. The project has been delayed due to progress reviews in services that support reviews, but remains programmed for action in 2023/24. Local rehabilitation services have worked closely with our Care at Home Service during the year to evolve service models focused on personal goals that involve delivering care and support with people rather than for people, where possible. Careful review of care packages has encouraged reablement and reduction in over-reliance on formal care. Weekly multidisciplinary meetings within our Home for Me Service allow for well-managed care and discharge planning resulting in over 85% of individuals requiring no further support at the end of 6-8 weeks. |
| Commitment: Supporting diversion from prosecution | |
| Extend the range of options for diversion from prosecution available to the Procurator Fiscal Service to extend ability to address the underlying causes of offending, as an alternative to prosecution (Improvement). |
Youth Justice team have had an increase in staff training in AIM3 which is a dynamic assessment model that helps practitioners to assess harmful sexual behaviours. This has supported more diversion reports from practitioners able to manage risks within the community. In 2022/23 the Social Work Justice Team has implemented new diversion guidance and extended diversion to ensure individual needs are met at the earliest opportunity, to enable people to desist from further crime. |
| Commitment: Improving school nursing services | |
| Develop School Nursing Services in line with “Transforming Nursing, Midwifery and Health Professions’ Roles: The school nursing role” (Improvement). | During 2022/23, the School Nursing Service delivered Lets Introduce Anxiety Management (LIAM) interventions as part of the development of enhanced support options. This was very successful, with a waiting list now in place due to demand. |
Our Performance
National Integration Indicators Used To Measure This Priority:
This section provides the HSCP’s performance against national core integration indicators:
RAG KEY:
 Positive performance improved in 2022/23
Positive performance improved in 2022/23 Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining
Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining
performance Performance declined in 2022/23
Performance declined in 2022/23
Other National and Local Indicators of Performance & Quality:
RAG KEY:
 On target
On target Within agreed variance of target
Within agreed variance of target Below Target
Below Target
| PI Title | 2022/23 | Note | |||
|---|---|---|---|---|---|
| Status | Value | Target | |||
| Prevention & Early Intervention | |||||
| % of customers (65+) meeting the target of 6 weeks from completion of community care assessment to service delivery |
|
97.6% | 95% | The national standard is to operate within a six week period from assessment to service delivery, which encourages efficiency and minimises delays for service-users. Aim = to maximise. | |
| % of CJSW Reports submitted to court by due date |  |
95% | 95% | National Outcomes & Standards (2010) states that the court will receive reports electronically from social work, no later than midday on the day before the court hearing. Aim = to maximise. | |
| The % of individuals beginning a work placement within 7 working days of receiving a Community Payback Order |  |
93% | 80% | The criminal justice social work service has responsibility for individuals subject to a Community Payback Order beginning a work placement within 7 days. Aim = to maximise. | |
| % of Court report requests allocated to a Social Worker within 2 Working Days of Receipt |  |
100% | 100% | National Outcomes & Standards (2010) places responsibility on the criminal justice service to provide an allocated criminal justice worker within 24 hours of the Court imposing a community sentence. Aim = to maximise. | |
Delivering our Key Social Work Public Protection Statutory Duties
| Our Highlights | |
|---|---|
| Increased delivery of Moving Forward Making Changes treatment programme for sex offenders, to reduce risk to the public. | Promotion of the ‘Safe and Together’ model which is designed to support victims of domestic violence and keep children safe and together with the protective parent. |
| Updating and implementing the new Child Protection Guidelines. | The implementation of the Violence and Sex Offenders register (VISOR) and associated procedures. |
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Prioritising public protection | |
| Ensure the highest quality standards in identifying and responding to actual and potential social work public protection concerns (Improvement). |
East Dunbartonshire HSCP ensures the highest quality standards in identifying and responding to actual and potential social work public protection concerns through the implementation this year of:
|
Our Performance
National Integration Indicators Used To Measure This Priority:
This section provides the HSCP’s performance against national core integration indicators:
RAG KEY:
 Positive performance improved in 2022/23
Positive performance improved in 2022/23 Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining
Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining
performance Performance declined in 2022/23
Performance declined in 2022/23
Other National and Local Indicators of Performance & Quality:
RAG KEY:
 On target
On target Within agreed variance of target
Within agreed variance of target Below Target
Below Target
|
PI Title |
2022/23 | note | ||
|---|---|---|---|---|
| Status | Value | Target | ||
| % of first Child Protection review case conferences taking place within 3 months of registration |  |
100% | 95% | Local standard and timescales set by East Dunbartonshire Child Protection Committee. Aim = to maximise |
| % of Adult Protection cases where the required timescales have been met |  |
94% | 92% | This indicator measures the speed with which sequential Adult Support and Protection actions are taken against timescales laid out in local social work procedures. Aim = to maximise |
| % of initial Child Protection Planning Meetings taking place within target timescale |  |
8890% | National targets have been changed during 2022/23 from 21 to 28 days. Target was achieved in three quarters out of four. A very small number of delays (<5) occurred in the April to June period that also caused the overall annual target to be missed. All were rescheduled to enable partner agency and parental attendance. Aim = to maximise |
|
| Percentage of first Review Child Protection Planning Meetings taking place within 6 months of registration |  |
100% | 95% | Local standard and timescales set by East Dunbartonshire Child Protection Committee. Aim = to maximise |
Supporting Families and Carers
| Our Highlights | |
|---|---|
| HSCP has reviewed, consulted on and updated its Carers Strategy for 2023-26, with supporting action plan. | The Promise Steering Group has implemented its action plan designed to improve outcomes for looked after children. |
| The HSCP Health Visiting Team received UNICEF Gold 4 Year Revalidation in 2022/23. | Delivery of Year 2 of the Children’s House Project has been completed, designed to improve the outcomes for care experienced young people moving on from care placements |
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Supporting carers with their own needs and in their caring role | |
| Recognise better the contribution of informal carers and families in keeping people safe and supporting them to continue to care if that is their choice (Improvement). |
East Dunbartonshire HSCP has consulted, reviewed and updated its Carers Strategy, which will be presented for approval to the HSCP Board in June 2023. This new strategy has been developed with the full involvement of carers, third sector partners and wider stakeholders. Our new Carers Strategy reflects the aspirations of the new national strategy but locates itself as an expression of local needs and priorities within East Dunbartonshire. When reviewing and updating the existing Adult Carer Support Plan, it was concluded that it didn’t fully capture personal outcomes. So the HSCP worked in partnership with Carers Link and a small group of Social Work practitioners to update the Adult Carers Support Plan, to more fully record personal outcomes. The group also developed a new Review document designed to report on the extent to which carers’ personal outcomes were being achieved, both informal and formal. |
| Commitment: Implementing The Promise for children and young people | |
| Ensure that every care experienced child grows up loved, safe and respected, able to realise their full potential (Improvement). |
The Promise Steering Group has implemented its action plan designed to improve outcomes for looked after children. This ensures that East Dunbartonshire HSCP is compliant with The Promise and its key principles are being embedded: (i) listening to children and young people, (ii) relationships, (iii) quality of care, (iv) sibling contact. The HSCP Health Visiting Team received UNICEF Gold 4 Year Revalidation in 2022/23. This award reflects standards designed to provide parents with the best possible care to build close and loving relationships with their baby and to feed their baby in ways which will support their health and development. However, ongoing resourcing issues in 2022/23 affected the Health Visiting team from fully implementing the Universal Health Visiting Pathway. |
| Commitment: Strengthening corporate parenting | |
| Strengthen corporate parenting, to improve longer term outcomes for care experienced young people, by community planning partners working collectively (Improvement). |
Delivery of Year 2 of Children’s House Project: The purpose of the house project is to improve outcomes for Care Experienced Young People moving on from care placements. There was a 100% success rate this year with 7 young people moving into their new homes. This was underpinned by strengthened links with the Council’s Housing Services to increase appropriate housing offers for care experienced young people. Other work in support of corporate parenting during 2022/23 included:
|
Our Performance
National Integration Indicators Used To Measure This Priority:
This section provides the HSCP’s performance against national core integration indicators:
RAG KEY:
 Positive performance improved in 2022/23
Positive performance improved in 2022/23
 Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining performance
Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining performance
 Performance declined in 2022/23
Performance declined in 2022/23
Other National and Local Indicators of Performance & Quality:
RAG KEY:
 On target
On target Within agreed variance of target
Within agreed variance of target Below Target
Below Target
| PI Title | 2022/23 | Note | ||
|---|---|---|---|---|
| Status | Value | Target | ||
| Percentage of child care Integrated Comprehensive Assessments (ICA) for Scottish Children’s Reporter Administration (SCRA) completed within target timescales (20 days), as per national target |  |
92% | 75% | This is a national target that is reported to SCRA and Scottish Government in accordance with time intervals monitoring. Aim = to maximise |
| Percentage of first Looked After & Accommodated reviews taking place within 4 weeks of the child being accommodated |  |
87% | 100% | National performance indicator. Subject to the impact of small numbers. Off target due to a small number of reviews (<5) outwith timescale, all to accommodate attendance by key personnel. Aim = to maximise |
| Balance of Care for looked after children: percentage of children being looked after in the Community |  |
83% | 89% | National performance indicator. Work continues to redress the balance of care by reviewing out of authority placements and continuing the Foster Carer recruitment campaign. Aim = to maximise |
| Percentage of children receiving 27-30 months assessment |  |
96.6% | 85% | This indicator relates to early identification of children with additional developmental needs and can then be referred to specialist services. Aim = to maximise |
Improving Mental Health and Recovery
| Our Highlights | |
|---|---|
| A wide range of improvements were achieved during 2022/23 to improve mental health services and support for children and young people. | Implementation of Medication Assisted Treatment (MAT) Standards, which promote safe, accessible and consistently high quality treatment for those affected by problematic drug use. |
| Agreement with the Mental Health Network and Scottish Drugs Foundation to work on a collaborative basis on local service user engagement | Highly successful joint working between the Community Mental Health Team and Alcohol and Drug Recovery Service on joint protocols and joint training initiatives |
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Improving adult mental health and alcohol and drugs recovery | |
| Redesign services for adult mental health and alcohol and drugs services to develop a recovery focussed approach (Redesign). |
The HSCP is reviewing the commissioned Mental Health and Alcohol & Drugs recovery services to develop enhanced, holistic recovery focused services across adult mental health and alcohol and drugs recovery. The HSCP has been unsuccessful in recruiting a Project Lead, which has delayed progress with this initiative. However, initial consultation and engagement sessions and Provider Forum led to agreement from Healthcare Improvement Scotland to support plans to take forward a Collaborative Commissioning model. Agreement was also reached with Mental Health Network and Scottish Drugs Foundation to work on a collaborative basis on local service user engagement. As part of our Drug Death Action Plan a focus of work has been to enhance joint working between the Community Mental Health Team and Alcohol and Drug Recovery Service. Joint protocols have been reviewed and updated and a series of joint training initiatives developed on trauma and substance misuse, motivational interviewing, children affected by substance misuse and ‘Staying Alive’. Extensive work has been undertaken during 2022/23 to implement Medication Assisted Treatment (MAT) standards, which ensure safe, accessible and consistently high-quality treatment for those affected by problematic drug use, to help reduce drug deaths and other harms and promote recovery The development of a new Mental Health Strategy commenced in 2022/23. |
| Commitment: Improving mental health support for children and young people | |
| The provision of faster, more responsive support for children and young people with mental health challenges (Improvement). |
A wide range of actions were undertaken during 2022/23 to improve mental health services and support for children and young people, including:
|
| Commitment: Improving post-diagnostic support for people with dementia | |
| Increase the capacity of the post diagnostic support service (Improvement). | The model for delivering Post Diagnostic Support has been reviewed and the service has been brought wholly in-house and additional hours added to the structure. It is expected that these changes will bring better performance in relation to people being seen within 12 weeks from their diagnosis. |
Our Performance
National and Local Indicators of Performance & Quality:
RAG KEY:
 On target
On target Within agreed variance of target
Within agreed variance of target Below Target
Below Target
| PI Title | 2022/23 | Note | ||
|---|---|---|---|---|
| Status | Value | Target | ||
| Improving Mental Health & Recovery | ||||
| Percentage of people waiting less than 18 weeks to start treatment for psychological therapies |  |
98.6% | 90% | This includes the Community, Primary and Older People’s Mental Health Teams. The service has delivered above target during 2022/23. Aim = to maximise. |
| Total number of Alcohol Brief Interventions delivered during the year |  |
332 | 487 | The delivery of ABIs has been below target since the onset of the pandemic. Recovery plans are in place including maximising digital technology and rebuilding capacity within GP surgeries. Aim = to maximise. Percentage of Young People seen or otherwise discharged from the CAMHS waiting list who had experienced a wait of less than 18 weeks 74.11% 90% Based on Q4 census |
| Percentage of Young People seen or otherwise discharged from the CAMHS waiting list who had experienced a wait of less than 18 weeks |  |
74.11% | 90% | Based on Q4 census period. The CAMHS service has substantially increased compliance with this standard, from 37% in Q1, but remains short of the national referral to treatment target. Aim = to maximise. |
| Percentage of People Waiting less than 3 weeks for Drug & Alcohol Treatment |  |
89.1% | 90% | Due to routine delays with data finalisation by Public Health Scotland, the figures here are for 2022 full calendar year. Performance is very marginally below 90% but within variance of 2% |
| Percentage of people newly diagnosed with dementia receiving Post Diagnostic Support (PDS) |  |
0% | 90% | In the early part of 2021/22, the service was operating almost at target levels, but became severely impacted by staffing issues that have persisted throughout 2022/23. The service has now moved over to a new operating model which should address performance issues. |
Post Pandemic Renewal
| Our Highlights | |
|---|---|
| Extensive impact assessment work undertaken to evaluate consequence of the pandemic on health and social care needs and complexity, to inform revised service models and approaches. | Successful phased approach to supporting staff safely back to the workplace, operating to a hybrid working pattern and in line with national guidance |
| Successful local clearing of the backlog of Community Payback Orders that had been suspended nationally in successive periods during lockdown | The HSCP Care Homes Support Team, working closely with local care homes, to ensure excellence in care and support for people living in this setting |
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Understanding and responding to the impact of the pandemic | |
| Understand the impact of the pandemic on the health and wellbeing of our population (including those living in care homes), the responses necessary to meet these needs and resource requirements (Redesign). |
Workforce Guidance within buildings has been aligned to a blended working approach where staff work both at home and in the workplace. This continued to be reviewed and changes to location of teams within building were put in place when necessary, to ensure maximum opportunities for integrated working. An Organisational Development plan was put in place to support staff returning to building based working arrangements with continued communication with staff throughout 2022/23. Staff are now working to respective partner blended working policies. Community Payback Orders During 2020-22 Covid-19 Testing Personal Protective Equipment Care Homes Support Team Analysis of Impact |
Our Performance
National and Local Indicators of Performance & Quality:
RAG KEY:
 On target
On target Within agreed variance of target
Within agreed variance of target Below Target
Below Target
| PI Titles | 2022/23 | Note | ||
|---|---|---|---|---|
| Status | Value | Target | ||
| Post Pandemic Renewal | ||||
| Reduction of Covid-19 backlog of Unpaid Work Orders (Outstanding Hours) | 5,578 hours | 5,578 hours | Backlog of Unpaid Work Orders due to the suspension of service during Covid-19 has been cleared within timescale. | |
Maximising Operational Integration
| Our Highlights | |
|---|---|
| The 2022/23 actions within the Joint Commissioning Plan for Unscheduled Care were successfully implemented, based on collaborative and innovative working practices. | Integrated quality management was further developed across the partnership, with enhanced oversight through clinical and care governance. |
| The HSCP evaluated its Adults with Incapacity practice. This led to an integrated action plan that is now being implemented across the HSCP. | The HSCP’s Vulnerable Pregnancy Process was reviewed and updated during 2022/23, leading to better information sharing and collaboration with Education Services and GPs. |
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Right Care Right Place: urgent and unscheduled health and social care redesign | |
| Improve patient experience, safety, clinical outcomes, and organisational efficiency in responding to and managing urgent health care needs and preventing unnecessary hospital care (Redesign). |
The 2022/23 actions within the Joint Commissioning Plan for unscheduled care were successfully implemented and included:
Hospital delayed discharge performance has fluctuated with significant challenges around placement to care homes in line with choice and affordability issues, and in meeting care at home demand in some areas. The HSCP’s Vulnerable Pregnancy Process was updated during 2022/23. The aim of this approach is to undertake holistic, person centred assessments for vulnerable pregnant women and unborn babies that will identify and minimise risk. Particular improvements have been made to information sharing and collaboration with Education Services and GPs. |
| Commitment: Developing integrated quality management arrangements | |
| Further develop robust, quality-driven clinical and care governance arrangements that reflect the National Health and Social Care Standards and the Partnership’s Quality Management Framework (Improvement). |
The HSCP’s Quality Management Framework was refreshed to reflect the impact of Covid-19 and a more robust connection to the Clinical & Care Governance Group was established. A new governance post was established and filled, to support the implementation of the HSCP Quality Management Framework. A new Self-Assessment Module was developed and piloted, that aims to strengthen team capacity for quality management and improvement action. This approach has been successful and will be rolled out to all teams and services during 2023/24, as part of the wider Performance Management Framework. The HSCP undertook a detailed self-evaluation of its practice with respect to Adults with Incapacity legislation and standards in 2022/23. The findings and analysis highlighted strengths in assessment and risk assessment, engagement with carers and families, application of legislation and appropriate use of powers. Areas for improvement identified were in relation to improving recording, consistent advocacy involvement, and establishing powers more proactively. An Improvement Action Plan is now taking forward these findings. The development of enhanced quality management has also been extended within Care at Home services and with new audit tools applied to Adult Community Nursing Services. |
Our Performance
National Integration Indicators Used To Measure This Priority:
This section provides the HSCP’s performance against national core integration indicators:
RAG KEY:
 Positive performance improved in 2022/23
Positive performance improved in 2022/23
 Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining performance
Performance steady (within 5% change in either direction). Arrow direction denotes improving/declining performance
 Performance declined in 2022/23
Performance declined in 2022/23
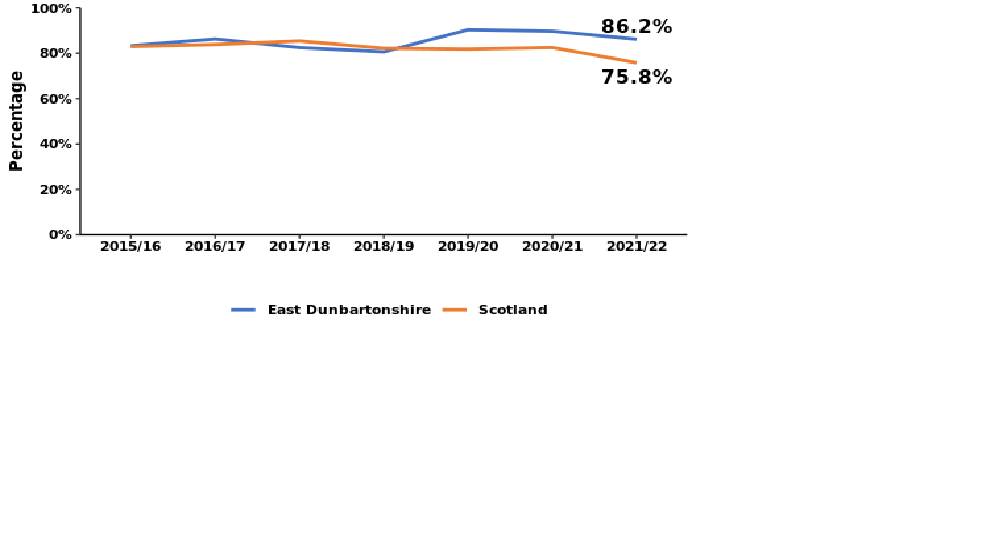
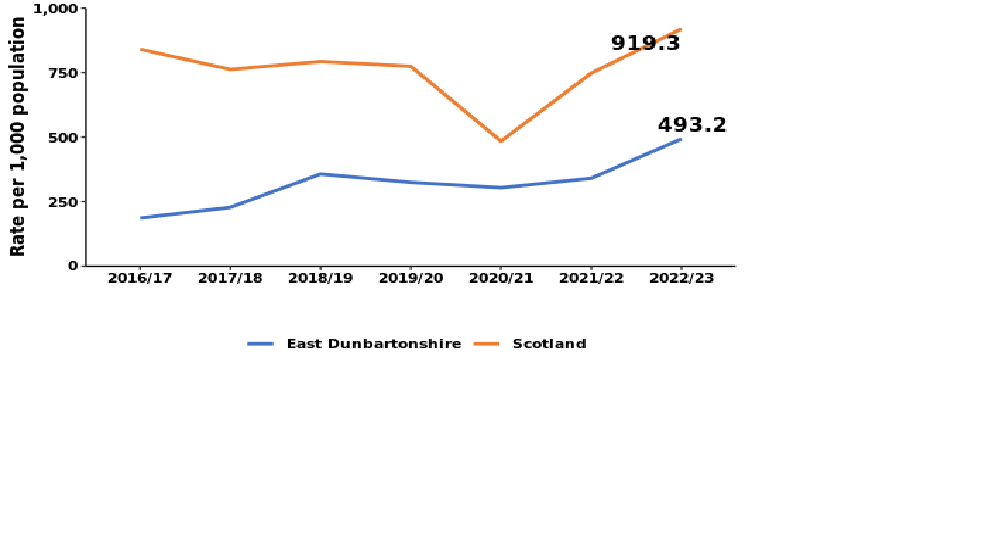
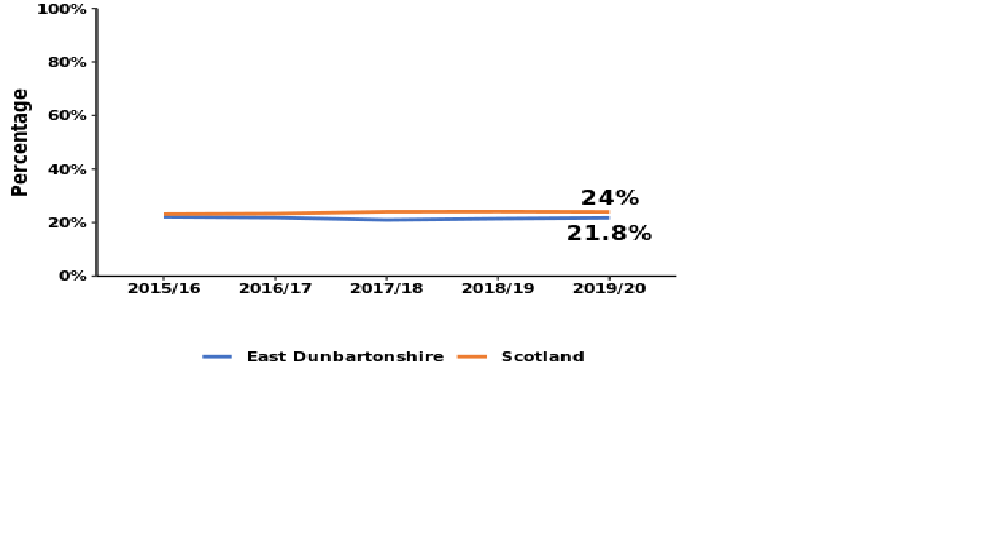
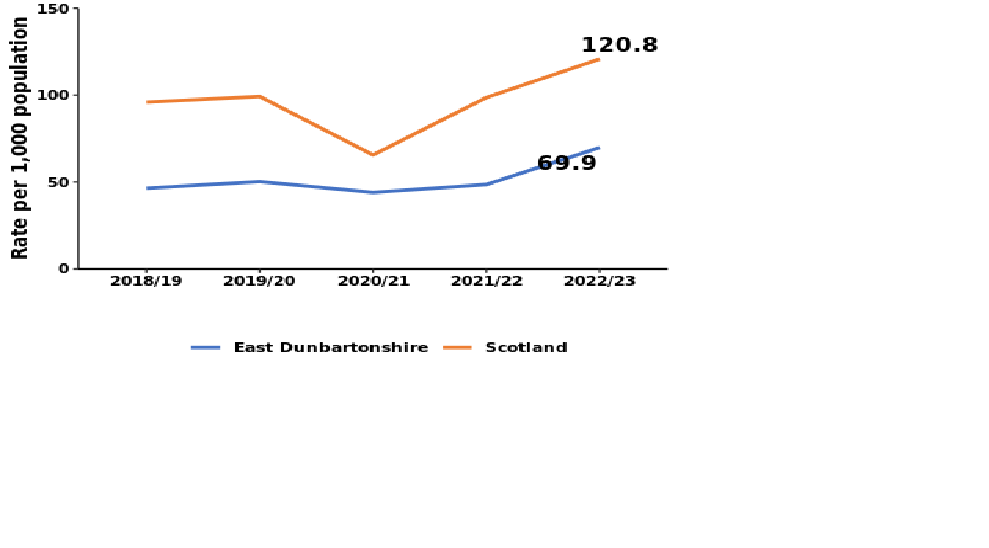
This section provides the HSCP’s performance against Scottish Government Ministerial Strategic Group (MSG) indicators
| Indicator and Rating | Performance Trend | |
|---|---|---|
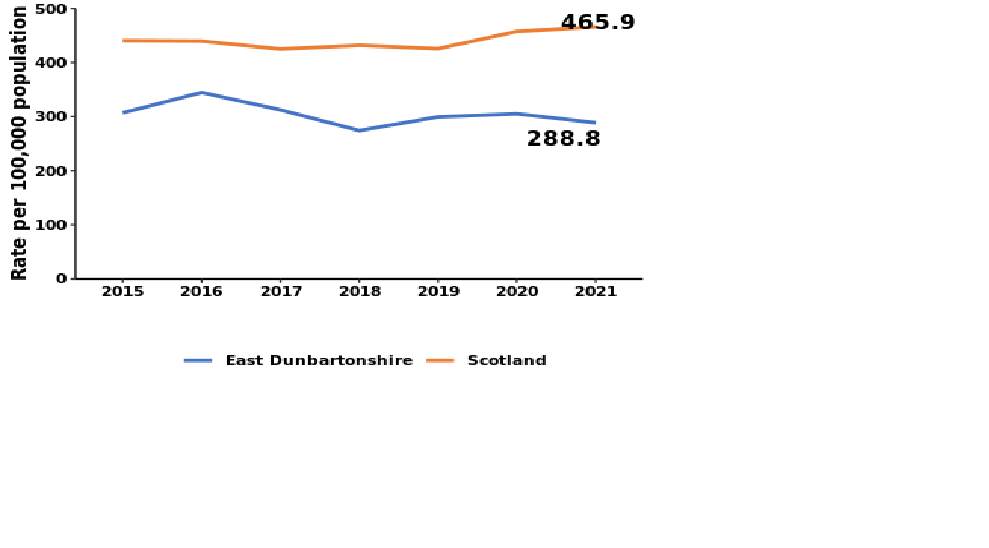
| 1. Unplanned admissions – rate per 1000 population (National Outcomes 1,2,3,4) (Objective: decrease) |
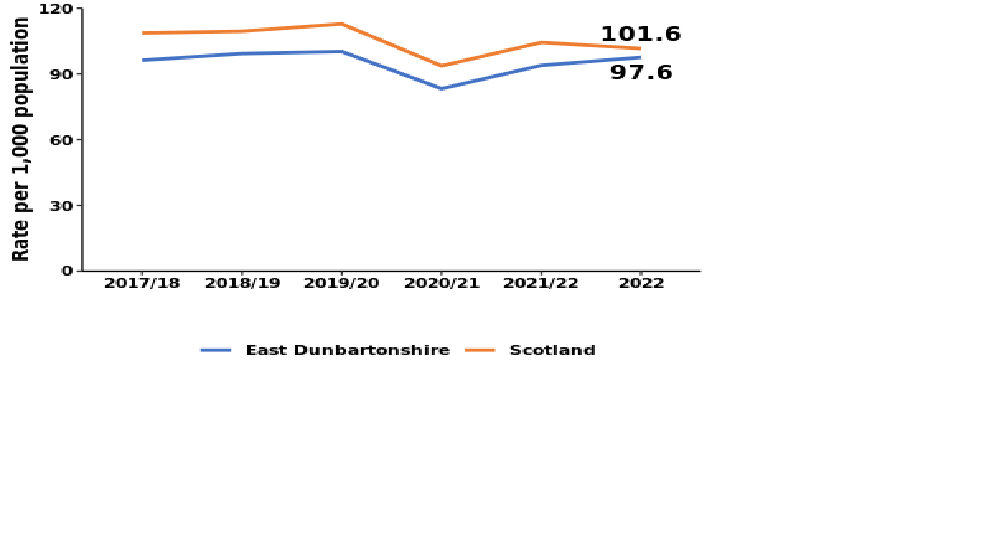 |
|
|
|
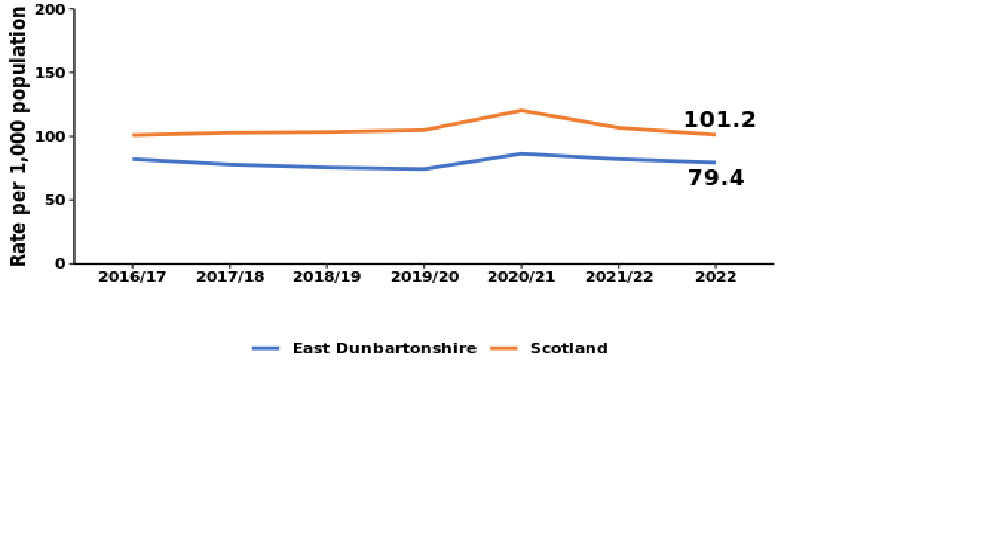
| Indicator | Performance Trend |
|---|---|
|
2. Unplanned bed days - rate per 1000 population (National Outcomes 2,4,7) |
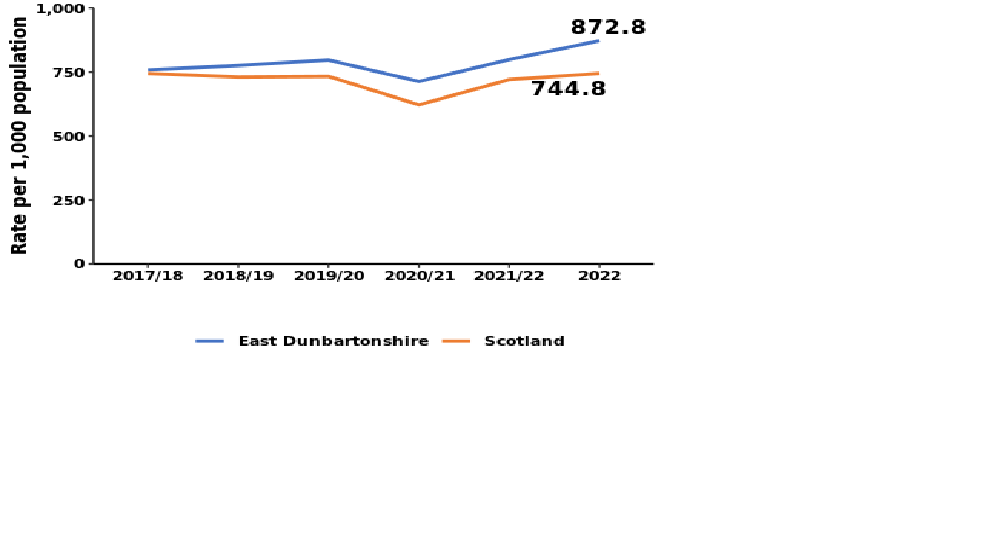 |
|
Performance behind Scottish average) |
|
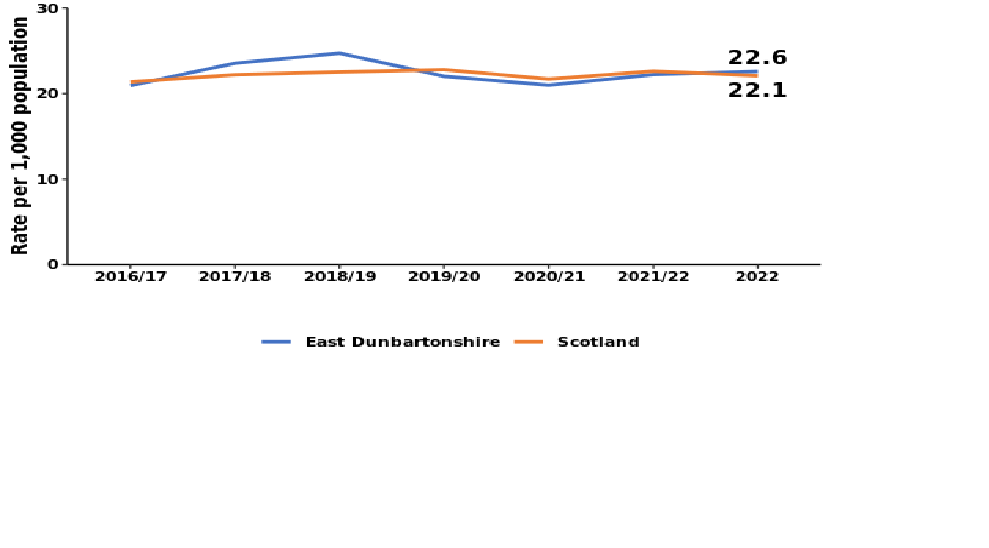
| 3. A&E attendances - rate per 1000 population (National Outcomes 1,2,9) (Objective: decrease) |
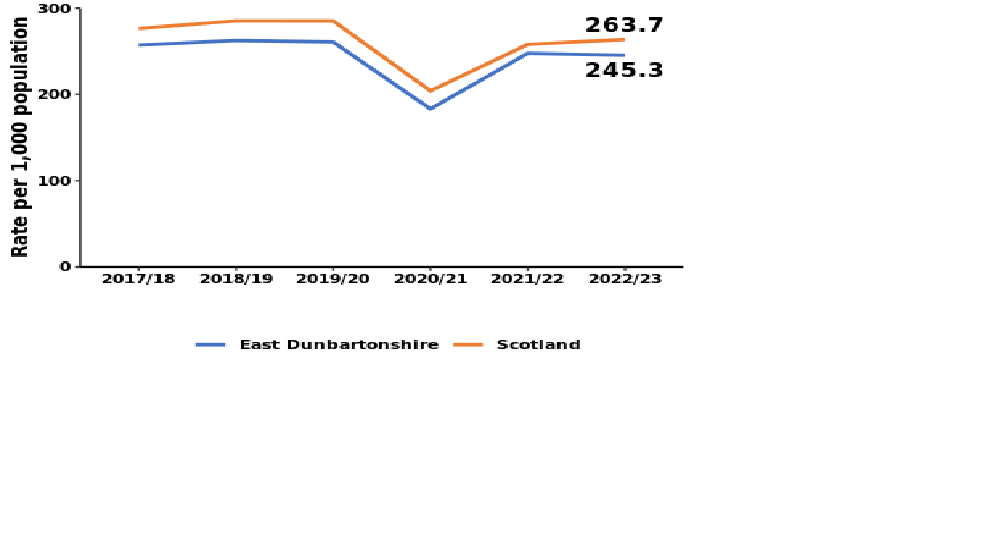 |
|
(Performance ahead of Scottish average) |
|
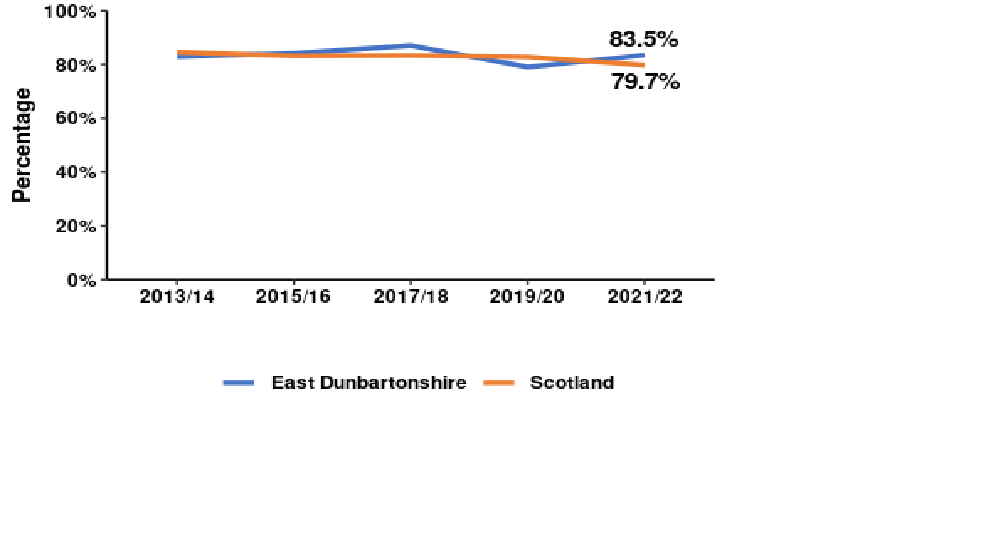
| 4. Admissions from A&E – rate per 1000 population (National Outcomes 1,2,3,4) (Objective: decrease) |
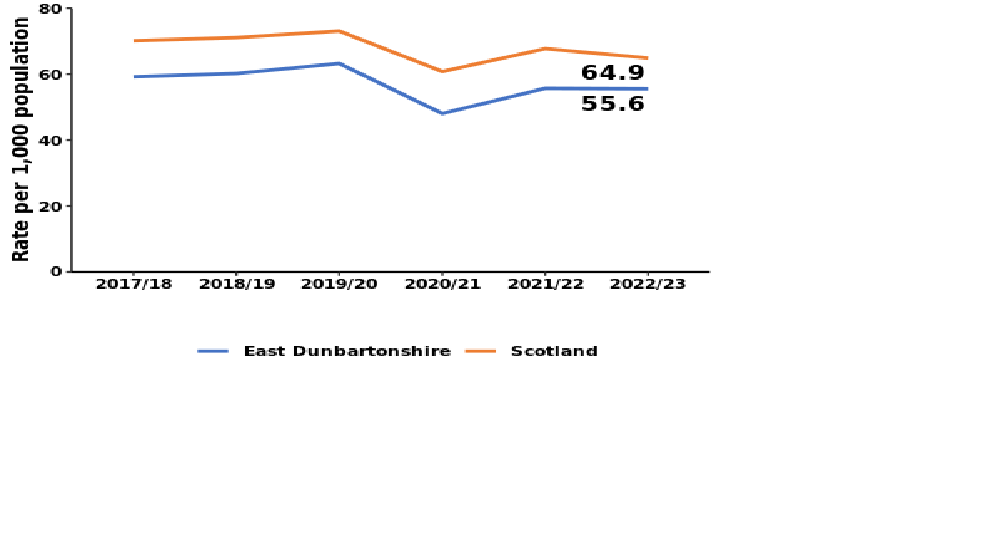 |
|
(Performance ahead of Scottish average) |
|
| 5. Delayed discharge bed days - rate per 1000 population (National Outcomes 2,3,4,9) (Objective: decrease) |
 |
|
(Performance ahead of Scottish average) |
How Well Are We Developing Our Enablers
This section of the Annual Performance Report sets out our progress towards the achievement of the enablers that underpin the priorities set out in our HSCP Strategic Plan and the associated national health and Wellbeing Outcomes
Workforce & Organisational Development
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Supporting the wellbeing of the health and social care workforce | |
| Respond to the pressures across all staff, independent contractors, commissioned services, partners and stakeholders due to the impact of the pandemic, with wellbeing support prioritised (Redesign). |
A range of measures have been developed and put in place to support staff wellbeing including:
|
| Commitment: Equipping the workforce and workplace during and after the pandemic | |
| Ensure that the workforce and the workplace is prepared and equipped to respond to the impact of the pandemic (Redesign). | During 2022/23, significant additional investment was made in core community health and social care services, and in adult social work. Capacity has improved across many areas of the HSCP functions, but persistent difficulties in recruiting to Social Worker, Mental Health Officer, Health Visiting and Social Care posts continues to present challenges. These challenges have impacted negatively on our capacity to respond to the level and complexity of presenting need. |
| Commitment: Redesigning the Public Dental Service | |
| Redesign the Public Dental Service by implementing a new service delivery model (Redesign). |
The redesign of the Public Dental Service to support the right care being delivered in the right place at the right time was significantly impacted by the pandemic and its impact on the services it provides. The recommendations have been reviewed in light of the changes that have been made to the Public Dental Service as a result of the pandemic and these recommendations will be implemented in 2023/24. |
| Commitment: Implementing a skills framework for supporting children’s mental health and wellbeing | |
| Support the improvement of children’s mental health and wellbeing, by implementing a national workforce knowledge and skills framework (Improvement). | The HSCP successfully completed Year 2 of the workforce knowledge and skills framework, notably establishing a Compassionate Distress Response Service and extending Lifelink Counselling. |
Medium Term Financial & Strategic Planning
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Maximising available resources | |
| Maximise available resources through efficiency, collaboration and integrated working (Improvement). |
The HSCP was able to manage service delivery within the budget set for 2022/23 in delivery of our strategic priorities. This included reporting on and maximising the funding available for specific priorities including the Primary Care Improvement Plan, Mental Health Action 15, Annual Delivery Plan, Mental Health Rapid Response (MHRRS) service and Adult Winter Planning. The HSCP aimed to increase adult social work capacity in line with the Scottish Government funding allocation and implement a revised operating model which is fit for purpose and aligned to the strategic priorities of the HSCP. Not all posts were filled as planned, due to resourcing issues within partner bodies to support job evaluation and recruitment. Work continue to progress these roles. |
| Commitment: Balancing investment and disinvestment | |
| Balance investment and disinvestment to deliver HSCP priorities within the medium term financial plan (Improvement). |
The IJB was able to set a balanced budget for 2023/24 in March which included a savings programme under written by general reserves to smooth in the delivery of key areas of disinvestment. Annual Delivery Plans are now developed each year to support the delivery of the HSCPs Strategic Plan priorities. These are underpinned by Head of Service Plans and Team Plans. The overarching planning, performance governance arrangements supporting these mechanisms are set out in a new HSCP Performance Management Framework. Successful redesign during 2022/23 in areas that aim to reduce overdependence on formal support, in support of more informal, rehabilitative and re-abling services demonstrate the work that the HSCP is doing to rebalance overall investment to deliver improved outcomes. This can also be demonstrated with the work undertaken to localise services to add value through improved integration and collaboration. |
| Commitment: Delivering financial sustainability | |
| Ensure longer term sustainability of services within available resources (Redesign) | The financial planning assumptions were updated for the next 5 years with work progressing to identify areas of service redesign which will deliver a balanced budget position for the HSCP going forward. |
Collaborative Commissioning and Whole System Working
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Co-designing solutions with the third and independent sectors | |
| Build collaborative commissioning through the development of improved efficiency, co-designed and co-produced solutions and better outcomes in collaboration with third and independent sector providers (Redesign). |
Collaborative commissioning approaches were introduced during 2022/23 in the areas of mental health services and alcohol and drugs services. This now provides a foundation for delivering this approach across other care groups and service areas. A review of the engagement framework used to support the HSCPs collaborative approach with the third and independent sector was undertaken and a new model has been designed, approved and implemented. |
| Commitment: Supporting primary care improvement | |
| Support primary care improvement and multi-disciplinary working through development in line with the new General Medical Services Contract Memorandum of Understanding (Improvement). | During 2022/23, the HSCP has continued with the implementation of the Primary Care Improvement Plan Memorandum of Understanding (2). Significant progress has been made. The HSCP is on track to complete a level of implementation deliverable within the current financial budget and with the limitations of accommodation and recruitment challenges. |
Infrastructure & Technology
Our Progress in 2022/23
| Objectives for 2022-25 | Progress in 2022/23 |
|---|---|
| Commitment: Modernising health and social care facilities | |
| Progress towards the development of appropriate, modern facilities that enable co-location of team members and services as well as alignment with GP Practices (Redesign). |
The HSCP has development a Property Strategy during 2022/23 which reflects and delivers on the priorities to support delivery of Primary Care Improvement Plan, wider HSCP property requirements and maximises opportunities related to hybrid working: An accommodation review progressed during 2022/23 with an expansion of space within Milngavie Enterprise Centre for office based staff previously located within Milngavie Clinic. This increases the opportunity to modernise clinical and therapeutic space close to local communities. Upgrades within the clinic have been completed during the year with more planned. A similar programme is underway within the East Locality, with shop-front premises secured in the Bishopbriggs area to convert into primary care clinical space. A review of the Woodlands Centre clinic and Kirkintilloch Health and Care Centre is also progressing with design plans developed to maximise clinical and therapeutic space within these buildings. Options are being reviewed to further expand clinical and drop-in space within the West Locality. A Health Board wide property evaluation during 2022/23 gave strong support to progressing an integrated health and social care solution within the West Locality; a business case will be developed and taken forward over the next year. |
| Commitment: Maximising the potential of digital solutions | |
| The delivery of a comprehensive Digital Health and Social Care Action Plan that maximises the potential of digital solutions, whilst ensuring equality of access for everyone (Redesign). |
The HSCP aims to implement its 2022/23 Digital Action Plan by 2024, which seeks to maximise experience of remote technology for a digitally enabled workforce, implement Analogue to Digital Telecare Transformation. Work towards Digital Maturity Assessment with the Scottish Government was not finalised due to delays within the Scottish Government and the loss of key information to inform the assessment. The HSCP is now participating in a national digital assessment of HSCPs. A number of local digital projects have concluded in the year, including “Ask Sara” which provides impartial advice about supportive equipment. |
Locality Planning
The HSCP established two Locality Planning Groups during 2015/16 to support the understanding, planning and delivery of services around communities within these localities. These locality areas relate to natural communities. They consist of:
- The east of East Dunbartonshire (Bishopbriggs, Torrance, Lenzie, Lennoxtown, and Kirkintilloch).
- The west of East Dunbartonshire (Bearsden and Milngavie).
The Locality Groups have brought together a range of stakeholders including GPs, social workers and social care professionals, community health professionals, carers and service users to facilitate an active role in, and to provide leadership for local planning of service provision.
Three Primary Care Clusters exist in Kirkintilloch and the Villages, Bishopbriggs and Auchinairn, and Bearsden and Milngavie. Most community health, social work and social care services are organised into either locality or cluster teams.
Locality Planning Groups: 2022/23 Update
The continued response to the pandemic had an impact on the impetus and delivery of the locality planning groups. Due to operational pressures, both groups were stood down for 2021/22 and 2022/23.
During this interim period, the HSCP has reviewed the leadership, membership, purpose and governance of locality planning within the HSCP, developing a revised model that ensures a closer link between locality needs, resources and assets.
The operational Locality Practitioner Collaborative model has continued to grow and develop in line with the increasing development of locality-based services and has now been implemented across the authority.
Core membership of the Locality Practitioner Collaboratives meets weekly and consists of senior practitioners from the East and West Social Work Teams, Community Occupational Therapy and Sensory Impairment Service, Community Rehabilitation Teams, Adult Community Nursing, Older People’s Mental Health Service and in-house Care at Home, with extended membership from Clinical and Primary Care Pharmacy Services, Adult Mental Health and Podiatry services.
The purpose of this weekly group is to discuss complex adult cases and utilise a Multi-Disciplinary Team approach involving collective knowledge, expertise and resources to improving outcomes for individuals and carers. This approach has shown that using a collective approach to supporting people with complex needs at home has enabled more to remain in their preferred place of care, with the right input to meet their needs. Feedback from the services involved has also been positive.
Building on the success of this approach, a Community Health and Care Services Locality Operational Leads Group was to be established in December 2022 with membership consisting of Team Leaders and Managers from the aforementioned teams meeting monthly. This arrangement has been designed to work alongside the establishment of an Extended Locality Collaborative, with wider membership from Children and Families, Adult Mental Health, Learning Disabilities, Public Health Improvement, Primary care and the Alcohol and Drugs Recovery Service which will meet quarterly. Due to the prolonged and particularly intensive winter pressure period, the establishment of these new collaborative groups was deferred until April 2023.
The Locality Planning Group meetings are also scheduled to re-launch in April/May 2023 where agreement will be reached on their future priorities and areas of focus. Budget has been set aside for both locality groups to facilitate small projects and direct engagement.
Hosted Services
Background and Context
The integration of services in a Health and Social Care Partnership involves a legal process whereby functions and services are delegated by the Council and Health Board to a separate governance body called an Integration Joint Board (IJB). In East Dunbartonshire, we call this our Health and Social Care Partnership Board. There are a range of services that by statute must be delegated to IJBs and there are additional functions and services that may be delegated.
For most services that are delegated to IJBs, these are arranged on a local area basis, so that each local IJB will oversee their strategy and operation as they are arranged and delivered for the area in which the IJB operates. There are six IJBs operating across the NHS Greater Glasgow and Clyde area, so that means that most services are split up into six divisions, one for each IJB. But some services cannot be easily split up, either because it would fragment the services or economies of scale would be lost. In these circumstances, it is often agreed that one IJB will “host” a service on behalf of some or all of the IJBs across the NHS Greater Glasgow and Clyde area.
East Dunbartonshire HSCP Board hosts two functions on behalf of the family of IJBs in the NHS Greater Glasgow and Clyde area: Specialist Children’s Services and Oral Health Services. These services are described in more detail below, with a summary of their achievements during 2022/23 and their planned priorities in the year ahead.
Specialist Children's Services (SCS)
Specialist Children’s Services (SCS) provide services to children and young people aged 0-18 with various long term, life limiting illness and disorders as well as mental health problems and difficulties. The total 0-18 year old population across the NHS Greater Glasgow and Clyde area is in excess of 215,000. In SCS, there are two overarching services: Child and Adolescent Mental Health Services (CAMHS) and Specialist Community Paediatrics Teams (SCPT), with our new Neurodevelopmental (ND) Service currently being piloted prior to NHS Greater Glasgow and Clyde Board-wide roll out.
SCS has a large workforce based throughout the NHS Greater Glasgow and Clyde area. Some of these staff work within the local communities such as health centres, in hospitals and inpatient units, schools – mainstream and additional support for learning schools and within the patient’s home and we have many office bases throughout the NHS Greater Glasgow and Clyde area.
Across Scotland, there is a tiered approach to mental health services in the public sector. GIRFEC principles underpin service delivery in each tier and these are built into service specifications. Tier 1 mental health support is delivered locally and as part of universal services such as Health Visiting and Education. Tier 2 covers mild mental health presentations and is targeted towards those who need it. These services are usually delivered by voluntary and community organisations and offer short term interventions. Tier 3 community CAMHS services are targeted at children and young people with moderate to severe mental health needs who require assessment, intervention and management which is more specialist than that which can be provide by universal services. Tier 4 CAMHS services focus on highly specialist services operating on a GGC level with small numbers of children who require specialist care. GGC CAMHS also host the regional child and adolescent psychiatric in-patient unit at Skye House, and one national service, the national children's psychiatric in-patient unit for under 12s at the Royal Hospital for Children.
Areas of Development and Progress during 2022/23
Over the last year, development and improvement work has predominantly focused on phase 1 of the Mental Health Recovery and Renewal plan, amongst other local run initiatives designed to improve services within SCS. Some highlights include:
- Implementation of the national CAMHS specification across Tier 3 and 4. CAMHS have been developing services towards each of the 7 national standards and the service is working towards auditing and reporting on these to evidence successful implementation.
- The expansion of some community CAMH services from an upper age limit of 18, up to 25 for specific targeted groups, most particularly care experienced young people. This development has also been put in place for our learning disabilities pathway with staff recruited to carry out this work.
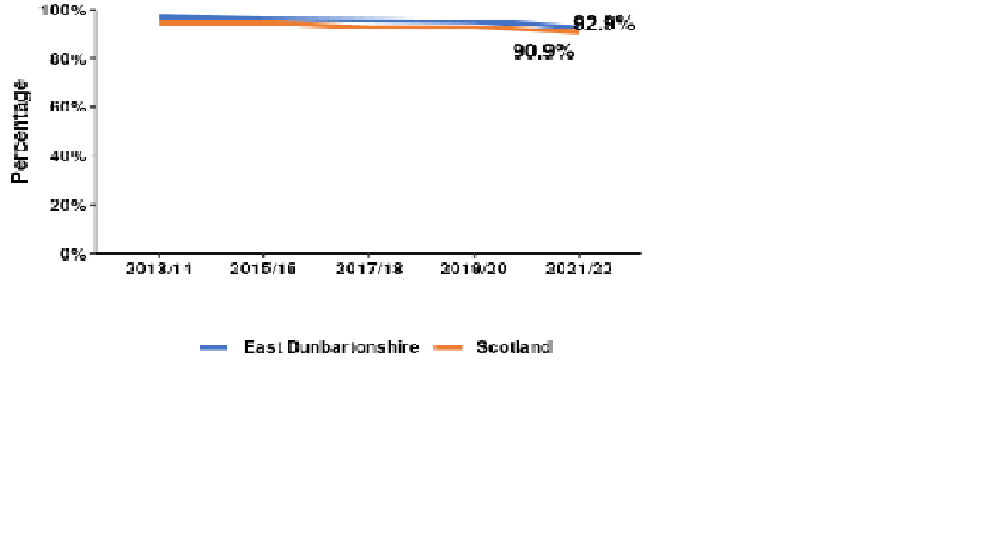
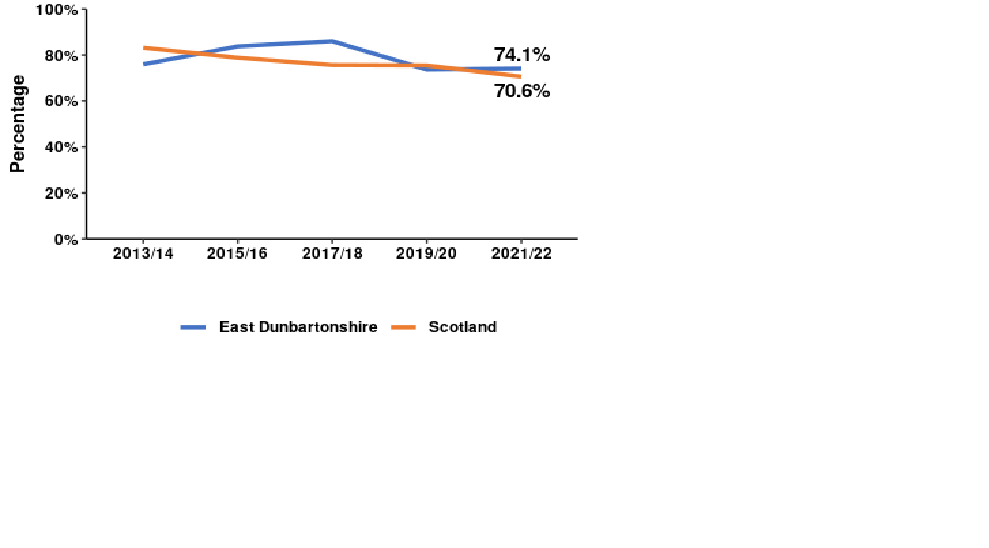
- The substantial reduction of waiting list backlogs for CAMHS. By the end of 2022/23, 74.1% of children / young people seen or otherwise discharged from the CAMHS waiting list had experienced a wait of less than 18 weeks. This is below the 90% national target but represents an improvement from the first quarter of 2022-23, when only 36.5% met the target.
Other work has been ongoing within phase 2 of the Mental Health Recovery and Renewal plan including the initial planning of a regional adolescent intensive psychiatric care unit, the improvement of CAMHS national data and the development of eating disorder services.
Areas for Focus during 2023/24
As part of the annual performance report and actions for the coming year, a series of development points linked to phase 2 of the Mental Health Recovery and Renewal plan will be important, alongside the ongoing effort for faster, more responsive support for children and young people.
We will continue to aim to meet the 18 week referral to treatment target to ensure children and young people are waiting less than 18 weeks. We will continue to focus on reducing the numbers waiting the longest. While the target has been met at the end of 2022/23 at a Health Board level, there are challenges in sustaining that performance linked to a combination of ongoing recruitment challenges and the need to balance offering first appointments to young people newly referred, with offering further follow up appointments to those already being seen. CAMHS will therefore aim to achieve and sustain this by the mid-point of 2023/24 with the longest waits being targeted each month to further reduce the length of waits. The workforce plan will be reviewed to focus on professional groups able to increase case holding capacity to create a larger core of nursing and psychology staff.
Alongside the implementation of the national CAMHS specification, the national children and young people’s Neurodevelopmental Specification will also be implemented throughout this year. This will create a third umbrella service across SCS, linking very closely with CAMHS and SCPT. The Neurodevelopmental Specification, along with clinical guidelines, a clinical competency framework and a demand and capacity model are all being developed for implementation. These are currently being piloted in two locality areas with the aim to roll out across NHS Greater Glasgow and Clyde, throughout the year.
SCS are working with Scottish Government, GGC eHealth and Public Health Scotland on the development of the Child, Adolescent and Psychological Therapies National Dataset (CAPTND), linking to all NHS Boards across Scotland. The aim is to improve the quantity and quality of monthly data submissions, alongside the improvement of data in general to support reporting on the national specifications. This work is underway and initial monitoring of improvements will be reported.
Oral Health Directorate
The Oral Health Directorate (OHD) is hosted within East Dunbartonshire Health and Social Care Partnership and has responsibility and accountability for Primary Care Dental services within NHS Greater Glasgow and Clyde (NHSGGC) Health Board. The responsibility and accountability for Secondary Care Dental services sits with the Regional Services Directorate, part of the Acute Sector of NHSGGC.
The OHD structure incorporates:
- General Dental Services including Greater Glasgow & Clyde Emergency Dental Service
- Public Dental Service
- Oral Health Improvement
- Secondary Care Dental Services
- Dental Public Health
General Dental Services (GDS)
The role of the OHD General Dental Services administration team is to provide a comprehensive administrative support service to 800 General Dental Practitioners in Greater Glasgow and Clyde in accordance with The National Health Services (General Dental Services) (Scotland) Regulations 2010. The department acts as an enabling function providing practitioners with the necessary support and expertise associated with their terms and conditions obligations. The department supports the organisation by ensuring that its statutory responsibilities are fulfilled in relation to this group of NHS independent contractors.
Public Dental Service (PDS)
The PDS service operates on a board-wide basis across 28 sites and provides comprehensive dental care and oral health education to priority group patients, including those with additional support needs, adult and paediatric learning disabilities, medically compromised and children who are unable to be seen routinely by GDS (these will include higher levels of treatment complexity and behavioural factors). Treatment is provided in clinics, schools and nurseries, care homes, outpatient daycentres, hospital settings, domiciliary visits, prisons and undergraduate outreach clinics.
Oral Health Improvement
Incorporating strategic and organisational leadership to reduce oral health inequalities, including fulfilling NHSGGC responsibilities in relation to the Oral Health Improvement Plan (2018), delivery of national Oral Health Programmes (such as Childsmile and Caring for Smiles), local oral health strategy and for oral health improvement requirements and ambitions across other programmes in NHSGGC.
Secondary Care Dental (SCD) Service
SCD services also known as Hospital Dental services are the main referral centre for specialist dental services for NHSGGC and the West of Scotland. SCD services accept patients on referral from medical and dental practitioners as well as tertiary referrals from other areas/specialties, including Emergency Dental Treatment Centre (EDTC) and the Out of Hours (OOH) service. Patients can be treated in outpatient clinics or, depending on the treatment required, patients are admitted as inpatients or day cases. Treatment is carried out in the Glasgow Dental Hospital (outpatients) as well as many hospital sites (inpatients/day cases) within the Acute Sector of NHSGGC.
Dental Public Health
Dental Public Health is the speciality of dentistry that deals with the prevention of oral disease, promotion of oral health and improvement of quality of life through the organised and collective efforts of society. Dental Public Health practitioners also have roles in health protection related to dentistry and provide strategic input to the management of healthcare services. The NHSGGC Consultant in Dental Public Health sits within the OHD and works alongside colleagues in the Public Health Directorate and Health Improvement in the Health Board and HSCP’s.
Areas of Development and Progress during 2022/23
Over the last year development and improvement work has predominantly focused on recovery of primary and secondary care dental services. Some highlights include:
- Resurrection of the Public Dental Service Review post pandemic and the creation of short life working groups to re-align the recommendations of the review in a post Covid era.
- Revalidation of Paediatric General Anaesthetic (GA) waiting lists to respond to waiting times challenges and deflect as may patients as possible who are awaiting GA to other appropriate modalities of care and treatment.
- Through non-recurring Winter Preparedness Funding (WPF) the PDS was able to increase access to routine dental care for patients within GGC. The funding was used to support access to emergency and urgent dental care and support patients who were not able to register with a dentist. A highlight was the PDS’s ability to respond to significant access issues within Inverclyde by creating an Access Centre. Furthermore, an occasional care clinic was set up to deliver emergency and routine dental services for patients referred by the EDTC and OOH clinics who could not access NHS dental care through their local general dental practitioner.
- The OHD stated a robust case and worked closely with Scottish Government to have Inverclyde (under the remote and rural label) included on the list of areas eligible to apply for financial incentives through the Scottish Dental Access Initiative. The initiative allows eligible practices/practitioners within the Inverclyde area to apply for the grant.
Areas for Focus during 2023/24
As part of the annual performance report for the coming year and in response expected changes within Dental Services in Scotland it is important for the OHD to focus on supporting access to NHS dentistry within Greater Glasgow and Clyde. We aim to scope and implement access initiatives throughout primary care oral health services. The key challenge is the awaited outcome of the Dental Reform process and the proposed Determination 1 of the Statement of Dental Remuneration.
Flexible implementation of the recommendations from the Public Dental Service review Programme Board are a key focus for 2023/24 with the creation of a work programme and key work streams alongside the appointment of a Programme Manager to support implementation within agreed timescales. Consideration needs to be given to the outcome of the review of the Statement of Dental Remuneration and the impact of Determination 1 on PDS services; this is expected in October 2023 and may result in changes or additionality to the recommendations in order to be responsive to PDS needs and protect its core services.
The creation and implementation of an OHD wide Communication and Engagement Strategy is a primary focus for the coming year. The initial focus will be establishing and capturing the OHD “audience” which spans both Primary and Secondary Care settings. The creation of a rolling communications programme and action plan that is meaningful to our audience and key stakeholders via social media and other mediums. The intention that by the end of the year the strategy will be embedded as business as usual.
Other Achievements and Good Practice Highlights
Each year we report on a wide range of achievements that have been delivered across the HSCP, many of which represent new and innovative ways of working. Managers and staff demonstrate good and improving practice in their day to day work and we feel it is important to showcase these:
Care About Physical Activity (CAPA):
Allied Health Professionals – Support to Care Homes
Care Home residents now have access to care and treatment when required by a Physiotherapist, Occupational Therapist or Senior Rehabilitation Worker, to support residents who have been discharged from hospital and who need support to improve their function or mobility, to remain as independent as possible as per the recommendations in the Scottish Government’s Care About Physical Activity Agenda.
Care About Physical Activity Projects
Two projects have been initiated by the CAPA team in line with the National Improvement Programme for Physical Activity Projects within two local Care Homes. Each project aimed to improve the amount of physical activities offered to residents and support Care Home Staff in delivering activities based on the resident’s interests and needs. Both have been a success and have encouraged residents to be more active, particularly male residents who had not previously been showing an interest in taking part in activities. These activities support the reduction and prevention of falls and improves the mental health of residents.
A new Care Home Activity Coordinators Peer Support Group has also been set up to enable Care Home staff to share ideas about what has worked well within their Care Homes in relation to increasing the physical activity of residents.
Falls Reduction
The CAPA team have been delivering awareness raising and training sessions to Care Home staff about the Falls Pathway. This approach supports good decision after a resident has fallen and provides staff with professional advice about alternatives to hospital attendance and potential admission.
UNICEF Baby Friendly Gold Award
The UNICEF UK Baby Friendly Initiative enables public services to better support families with feeding and developing close and loving relationships, so that all babies get the best possible start in life. The Health Visiting Service were awarded a UNICEF Baby Friendly gold award in November 2022.
District Nursing Service
Extension of Core Hours
After consultation and a test of change, the District Nursing Service implemented a new working-hours model in September 2023 to provide core services to patients between 08:30 and 22:00, 7 days a week. This new model has shown significant improvements in patient experience, particularly for palliative care, with timely responses to unplanned visits, better continuity of visits and improved communication across the service.
Quality Assurance
A new Quality Assurance audit has been implemented within the District Nursing service. This monthly audit includes in-depth exploration of nursing clinical records and shadowing to include qualitative and quantitative outcomes. Since June 2022, all three District Nursing teams have achieved a consistent Gold rating which is 90% compliance and over and demonstrates a high standard of care across the whole service.
Children’s Mental Health and Emotional Wellbeing
During the pandemic the numbers of children and young people seeking support for anxiety and eating disorders increased significantly. In response, our Delivering for Children and Young People Partnership (DCYPP) prioritised improvements in this area. The aim has been to improve early access to mental health, wellbeing and emotional support that is fit for purpose, at the right time and in the right place. New funding has been used to develop local pilot projects, including a Compassionate Distress Response Service (aged 16-26) and additional counselling provided by LifeLink to support home schooled children and young people 16+ who are not in school. This service specifically targeted young people referred for support to the Children & Young People Mental Health Services (CAMHS).
Wayfinder – Peer Navigator for Justice Clients
Working in collaboration with the Alcohol and Drug Partnership and the Community Justice Partnership, Justice Social Work services secured funding from the Drugs Death Task Force, to commission a Peer Navigator post to enhance justice clients’ ability to access alcohol and drugs services with a view to improving outcomes and reducing drug deaths.
The Peer Navigator has lived expertise and uses relationship-based practice to develop supportive and meaningful relationships with clients, many of whom are often difficult to engage. This service is aimed at men subject to community-based disposals and those returning to the community after custodial sentences.
Since coming into post the navigator has supported 15 clients to positive destinations.
Connect-ED
Connect-ED was an initiative piloted during 2022/23 to promote healthy aging and independence. It delivered a range of health and wellbeing information and support from the HSCP, the Council and local third sector services.
During the 6-month programme, 59 people were supported on issues including Power of Attorney and wills advice, provided by our Age Scotland partner. Others were provided with information on social clubs, walking groups and enquired about volunteering opportunities. It is also notable that all organisations who took part in the programme reported increased referrals and established new networks.
Mind of My Own App
The child care Integrated Comprehensive Assessment (ICA) cannot be completed and authorised for the Scottish Children’s Reporter if the Child/Parents view is not recorded. In response to this, the Children and Families team have introduced the Mind of My Own App, which enables children and young people to communicate their views, experiences and feelings to a trusted adult in a safe digital space. This supports practitioner in understanding the child or young person, enables them to respond quickly to them and evidences their views.
Income Maximisation
In 2022 the Health Improvement Team devised and developed a digital QR code to support the Income Maximisation service. The service can now receive service user referrals directly from the new digital pathway incorporating a quicker self-referral route, streamlining the process and making the service more accessible for a wider range of individuals.
East Dunbartonshire Improving the Cancer Journey
This service, in partnership with Macmillan Cancer Support has been running for 16 months and helps people to get the support they need, whether that's physical, emotional, practical, medical or financial. In 2022 the service entered into partnership with Low Moss Prison to offer the service to those who live or work within the prison environment. This partnership is being cited as an area of good practice by both the Scottish Prison Service and The Scottish Government.
Children and Young People’s Mental Health
The School Nursing service continues to support the increasing number of children and young people seeking support for mental health and wellbeing. Through training and development, the team have upskilled staff to support children and young people with complex health needs and/or emotional health and wellbeing needs. All school nurses provide Lets Introduce Anxiety Management (LIAM) intervention to 8-18 years.
Access to Advanced Practitioner – Festive Holiday Cover
Advanced Nurse Practitioner access was arranged over the 4 public holidays during the festive period to give advanced support to four care homes that were in a Covid-19 outbreak at the time as well as support to patients in their own home. Within the care homes, this resulted in 21 calls to NHS24 or GP Out of Hours being avoided as well as 12 potential hospital admissions being avoided. For those patients at home, 6 potential hospital admissions and 10 calls to GP Out of Hours were avoided.
Perinatal Mental Health Services
The Enjoy Your Baby Group has been expanded to included fathers and partners as well as mothers. It is an evidence-based programme for the management of stress, anxiety and depression for parents experiencing mild to moderate mental health challenges, during this period. The programme promotes early intervention, reducing the risk of deterioration using a recovery-based model of person-centred care, taking account of the parent’s needs and that of their infant, partner and family.
Care Home Support Team
Anticipatory Care Planning (ACPs)
The Care Home Liaison nurses are promoting the importance of Anticipatory Care Planning for care home residents which is a plan for how and where they would like to be cared in the future and identifies what personal outcomes are important to that individual. This information is available on a shared electronic system accessed by the ambulance service, GPs and health staff working within community and Acute services. Anticipatory Care Plans enable a meaningful conversation with residents about preferred place of care and contribute to the reduction of unscheduled admissions and the facilitation of successful and timely discharge from hospital. Education has been provided to the whole team and to the community social work teams.
Project Milkshake
The Dietitian, in conjunction with the Care Home Dietetic team (Health Board wide), started a pilot project during 2022/23, Project Milkshake, within one East Dunbartonshire care home that promotes the use of milkshakes and a ‘Food First’ approach for residents experiencing weight loss.
Relatives Forum
In collaboration with Carers Link, a Relatives Forum has been established for relatives of care home residents with an emphasis on mutual support. Topics that have or will be covered include food, fluid and nutrition, bereavement, finances, meaningful / physical activities, life story work, palliative care and anticipatory care planning.
Community Mental Health Team
Attention Deficit Hyperactivity Disorder (ADHD)
During 2022/23 a new ADHD assessment clinic was established on a Saturday to enable people to attend out with working or school hours. This is proving popular with clinic attendance rates at 100%.
Public Dental Service
The Public Dental Service set up additional clinics in 2022/23 to tackle issues relating to reduced access to dental services experienced since the Covid-19 pandemic, in particular in General Dental Services. A Paediatric clinic has been set up to assess and treat children who have been unable to access routine dental care within General Dental Practice. A service for frail elderly patients has been established for patients who require routine domiciliary care but do not need input from the Special Care Dental Team. An occasional clinic has also been established to offer a single course of treatment for unregistered patients who required a course of dental care to secure oral health but were unable to register with a General Dental Practice due to ongoing access issues.
“Make it Work”
Having a job is considered to be one of the main positive influences on an individual’s ability to not reoffend. It not only improves their prospects of securing appropriate accommodation, healthcare, and more secure finances, but it can provide them with new peer groups, and help build their resilience and a positive self-image.
In collaboration with the Local Employability Partnership (LEP) the Community Justice team have introduced the ‘Make it Work’ East Dunbartonshire employability project for people in contact with the Justice system.
A dedicated employment advisor has been employed and 21 people started on the first year of the programme in 2022/23, with 14 gaining a qualification necessary for ongoing employment and 9 people starting employment.
Electronic Medical Administration Record (eMAR)
eMAR is an electronic medical records software which is an alternative to the paper-based Medical Administration (MAR) sheets used for managing medication administration. The HSCP Care at Home team are currently piloting eMAR through their scheduling system, with a small number of clients who are receiving prescribed creams in conjunction with the District Nursing Service. This enables the Care at Home Carers to apply the prescribed cream based on the scheduling and dosages entered by the District Nurses. The hope is that the eMAR system can be rolled out to a great number of customers for a wider number of prescribed medications in the future.
Home & Mobile Health Monitoring for Self-Management
Blood Pressure Monitoring
Blood pressure monitors have been distributed across 6 GP Practices involved in the rollout of the self-management of blood pressure monitoring. 176 patients so far are monitoring their blood pressure at home preventing repeat visits to their GP practice.
Community Treatment and Care Service (CTAC) - Vitamin B12 Injections
Patients have fed back to the CTAC team that for some of them, having to attend regular clinic appointments for their Vitamin B12 injections was negatively impacting on their life due to the time it took to attend appointments. This feedback led the team to introduce a test of change for interested patients which focused on developing training resources to support and educate willing participants to self-administer vitamin B12 injections. The pilot was launched successfully in March 23 with 16 service users now self-managing their condition. A further 30 service users have expressed an interest in undertaking the training to allow them to self-manage their condition.
Rehabilitation
Home For Me
The Home For Me service is a continuously developing joint service between the Community Rehabilitation Team and the Care at Home service. These services work jointly to provide a short period of rehabilitation and reablement to promote independence and reduce the need for an ongoing care package. The majority of service users have had a recent hospital admission and a change in their functional abilities.
This collaborative way of working allows individuals to receive care when required, whilst receiving rehabilitation, setting patient centred goals and reducing their reliance on services. The service has also been used to prevent admission to hospital where a short term packages of care has been put in place to support someone at home during a period of ill health. Currently the service manages to support 93% of individuals back to full independence. Customer feedback has been very positive.
Frailty Practitioners
East Dunbartonshire HSCP now has 2 Frailty Practitioner posts within the Community Rehab Team as part of a wider NHS Greater Glasgow & Clyde response to the issue of frailty across the Health Board area. The Frailty Practitioners provide a comprehensive assessment of individuals identified as living with frailty within the community.
Work has also commenced with 2 GP practices to identify individuals in the community who would benefit from a comprehensive assessment within their own home. They will then receive advice for self-management of any issues they may have been having, sign-posting to any supports they may need and/or a referral to any professional services they may require.
“Apna Ghar”
Apna Ghar is a new group within the Bearsden area for women from ethnic minority backgrounds. The group offers a friendly, welcoming environment, encouraging friendship and peer support.
The Older People Local Area Co-ordination Service worked in partnership with the volunteers and organiser for the group, East Dunbartonshire Voluntary Action (EDVA), the public and the Council to establish the group, secure accommodation, develop the group’s constitution and membership, and support funding applications. The group now operates independently with minimal ongoing assistance from the Local Area Co-ordination Team.
Alcohol and Drugs Recovery Service
The Alcohol and Drugs Recovery Service has developed a new Standard Operating Procedure that the Scottish Government are utilising as an example of good practice and sharing with other Alcohol and Drug Partnership areas.
AskSARA is a self-help website which gives impartial expert advice and information on products and equipment to help make daily living easier for older and disabled people. The HSCP continues to promote and raise awareness of the AskSARA service. There has been a 33% increase in activity from last year.
Engagement with Place Communities
During the past year, the HSCP has been working in partnership with our community planning partners to consult with the communities in Lennoxtown, Hillhead and Harestanes, Twechar and Auchinairn. The consultation was undertaken to inform the new Locality Plans which will drive work in those areas and will replace the previous Place plans.
During the consultation, the Public Health Improvement Team engaged with approximately 420 people to find out what support they need as we work through and out of the pandemic and how we can help empower communities to support themselves in a true community-led approach.
This partnership approach has helped build and maintain stronger relationships between partners in East Dunbartonshire, share resources and skills and lead to a more joined up and community-led approach.
Income Maximisation
Over the past 5 years the Income Maximisation Service has generated a total of £3,898,000 of income which has directly benefited East Dunbartonshire residents. This service which is managed by the Public Health Improvement Team (HIT), supports the HSCPs ambition to mitigate poverty and increase health & wellbeing outcomes across East Dunbartonshire. In 2022 the HIT added a digital QR code to support referral to the income maximisation service. This has helped to streamline and simplifying the referral process, reducing barriers and widening its reach.
Trauma Informed Practice
A number of the teams across the HSCP have invested significantly in embedding trauma informed practice during 2022/23, recognising where people are affected by trauma and adversity, and better able to respond in ways that prevent further harm and support recovery. Staff training has been rolled out and work has begun to improve clinical spaces to appear more user friendly with framed pictures, furnishings and softer lighting. Noise outside rooms has also reduced by minimising staff use of the corridors. In November 2022 we appointed a Trauma Informed Coordinator to progress this work and support the Aces and Trauma Collaborative.
Joint Learning Disability Services
In line with Scotland’s National Dementia Strategy, the team has been contributing towards the development of dementia support for people with learning disabilities. We have contributed towards the development of a new care plan guidance resource for Post Diagnostic Support. We have also been involved in the development and delivery of a dementia training programme, in line with the ‘Promoting Excellence’ framework, which is being rolled out across NHS GG&C Learning Disability Services.
Financial Performance
Financial Performance 2022/23
The partnership’s financial performance is presented in the Annual Accounts. The Comprehensive Income and Expenditure Statement (CIES) describes expenditure and income by care group across the IJB and shows an over spend of £6.928m
against the partnership funding available for 2022/23. Adjusting this position for in year movements in reserves provides an underlying positive variance on budget of £4.387m for 2022/23 which represents operational service delivery for the year and
has been reported throughout the year to the IJB through regular revenue monitoring updates.
This has reduced the overall reserves position for the HSCP from a balance of £26.990m at the year ending 31 March 2022 to that of a balance of £20.062m as at year ending 31 March 2023. The reserves can be broken down as follows:
The CIES includes £2.930m of expenditure related to the impact from Covid-19. The costs incurred during 2022/23 are set out in the table below.
| Additional Covid-19 Costs - HSCP513 | 2022-23 Revenue Total |
|---|---|
| Flu Vaccination & Covid-19 Vaccination (FVCV) | 181,186 |
| Additional Staff Costs (Contracted staff) | 239,379 |
| Additional Staff Costs (Non-contracted staff) | 57,374 |
| Additional Equipment and Maintenance | 513 |
| Additional PPE | 30,321 |
| Additional Capacity in Community | 140,547 |
| Children and Family Services | 895,242 |
| Covid-19 Financial Support for Adult Social Care Providers | 1,167,495 |
| Additional FHS Contractor Costs | 72,322 |
| Digital & IT costs | 4,086 |
| Loss of Income | 141,237 |
| Total Covid Costs - HSCP - All | 2,929,701 |
Costs were covered through HSCP earmarked reserves, held for this specific purpose. The balance of reserves of £7.034m was returned to SG in the financial year to be redistributed across the sector to meet current Covid-19 priorities. The mechanism by which the funds were returned resulted in the contribution from NHSGG&C being reduced by this amount.
Financial Outturn Position 2022/23
The budget for East Dunbartonshire HSCP was approved by the IJB on the 24th March 2022.This provided a total net budget for the year of £199.034m (including £38.514m related to the set aside budget). This included £0.449m of agreed savings to be delivered through efficiencies, service redesign and transformation to deliver a balanced budget for the year and moving forward into future years.
There have been a number of adjustments to the budget since the HSCP Board in March 2022 which has increased the annual budget for 22/23 to £208.479m. These adjustments relate mainly to non-recurring funding from SG specific to the dental health bundle, family health services, PCIP, ADP and the pay award for NHS and social work staff. This is netted off against the reduction in the NHS contribution related to the return of Covid funding in year.
The partnership’s financial performance across care groups is represented below:
| Care Group Analysis | Annual Budget 2022/23 £000 |
Annual Expenditure 2022/23 £000 |
Year End Variance £000 |
|---|---|---|---|
| Strategic & Resources | 4,615 | 4,465 | 149 |
| Older People & Adult Community Services | 52,188 | 48,793 | 3,395 |
| Physical Disability | 5,314 | 5,093 | 221 |
| Learning Disability | 22,859 | 23,142 | (283) |
| Mental Health | 4,363 | 4,501 | (138) |
| Addictions | 1,916 | 1,307 | 609 |
| Planning & Health Improvement | 618 | 552 | 66 |
| Children's Services | 15,632 | 14,930 | 702 |
| Criminal Justice Services | 416 | 455 | (39) |
| Other Non Social Work Services | 1,258 | 950 | 308 |
| Family Health Services | 33,220 | 33,218 | 2 |
| Prescribing | 21,095 | 22,027 | (932) |
| Oral Health Services | 11,713 | 12,738 | (1,025) |
| Set aside | 40,306 | 40,306 | 0 |
| Covid Expenditure | (7,034) | 2,930 | (9,964) |
| Net Expenditure | 208,479 | 215,407 | (6,928) |
A breakdown of the projected underspend against the allocation from each partner agency is set out in the table below:
| Partner agency | Annual Budget 2022/23 £000 |
Actual Expenditure 2022/23 £000 |
Year End Variance 22/23 £000 |
| East Dunbartonshire Council | 71,437 | 77,737 | (6,301) |
| NHS GG&C | 137,042 | 137,670 | (628) |
| Total | 208,479 | 215,407 | (6,928) |
The main reasons for the variances to budget for the HSCP during the year are set out below:
- Mental Health, Learning Disability, Addiction Services, Health Improvement (£0.255m under spend) - the overall variance relates to pressures in relation to increased taxi provision (as opposed to use of fleet transport) to support SW service users to access services, loss of income from charging due to numbers attending day services and in receipt of non-residential services not resuming to pre covid levels. This is offset by the numbers of care packages not resuming to pre covid levels anticipated at the time of setting the Budget for 2022/23, vacancies, ongoing recruitment and retention issues across nursing and psychology posts within MH and LD health services.
- Community Health and Care Services – Older People / Physical Disability (underspend of £3.616m) – there continued to be reduced levels of care home placements, supported living packages and care at home services purchased from the external market from that assumed at the time of setting the budget, due to the continuing impacts of Covid-19. Numbers are continuing to recover to more normalised levels. This mitigates pressures within the in-house care at home service and pressures in relation to equipment to support people to remain at home along with additional adult winter planning funding to increase capacity in this area. SG funding was made available in year for Adult winter planning which was not fully spent in year due to ongoing recruitment challenges in filling posts. This will be taken to earmarked reserves.
This also includes the refund of monies of £1.1m related to charges for continuing care beds within Fourhills Care Home dating back to 1st April 2019 (£0.3m related to 19/20, £0.4m related to 20/21 and £0.4m related to 21/22). - Children and Criminal Justice Services (underspend of £0.663m) – there continued to be recruitment and retention challenges across Children’s services for the year. There was also reductions in external fostering and residential childcare placements as children move onto positive destinations. There continue to be pressures in relation to Unaccompanied Asylum Seeking Children (USAC) where placements within in house provision is at capacity and will require the purchase of externally purchased placements to accommodate these children.
- Housing Aids and Adaptations and Care of Gardens (underspend of £0.308m) - there are a number of other budgets delegated to the HSCP related to private sector housing grants, care of gardens and fleet provision. These services are .delivered within the Council through the Place, Neighbourhood and Corporate Assets Directorate – there has been a continuing underspend in relation to fleet recharges related to a downturn in transport provision needed as a consequence of Covid and a reduction in services requiring this type of transport. This is compounded by underspends across the care and repair service and private sector housing grants.
- Prescribing (overspend of £0.932m) - pressures in relation to price and volume increases across a range of medicines have been reported throughout the financial year which has resulted in an adverse variance in this area. A number of initiatives are in development to target the volume and types of prescriptions dispensed such as script-switch, review of use of formulary vs non formulary, waste reduction, repeat prescription practices. Prices across the market will continue due to global factors outwith the control of the HSCP, however use of alternative medicines will form part of the programme of initiatives being rolled out across East Dunbartonshire and more widely across GG&C.
- Oral Health (overspend of £1.025m) - the overspend relates to expenditure incurred in year on temporary staffing to address winter pressures and ventilation and equipment purchases in support of recovery of services following the pandemic to be funded from earmarked reserves set aside for this purpose. This was offset by some delays in filling vacancies during the year.
- Covid Expenditure (overspend of £9.964m) – there was expenditure related to Covid-19 during the year of £2.930m and the return of un-used reserves to SG of £7.034m. This expenditure will be met entirely from HSCP earmarked reserves held for this purpose.
Partnership Reserves
As at the 1 April 2022, the HSCP had a general (contingency) reserves balance of £3.1m. The surplus on operational service delivery generated during 2022/23 (£4.387m) will allow the HSCP to further that reserve in line with the HSCP Reserves Policy. This will provide the HSCP with some financial sustainability into future years and an ability to manage in year unplanned events and afford a contingency to manage budget pressures without the need to resort to additional partner contributions as a means of delivering a balanced budget.
The performance of the budget during 2022/23 supports the HSCP in the enhancement of a reserve to support the redesign of accommodation by a further £1m. This will increase the reserve already available to £3m to support the HSCP in delivery of its strategic priorities, primarily related to the delivery of the primary care improvement programme, moving services currently delivered within acute settings to local communities, such as Phlebotomy, and additional space to accommodate increased staffing capacity in response to Adult Winter Planning monies, adult social work capacity funding. In addition it will facilitate the creation of a digital redesign programme of £0.5m in response to the outcome of a national digital maturity assessment and the work already underway as a result of the Covid-19 pandemic where resort to digital platforms moved forward significantly and needs ongoing investment to maintain and develop further. At its meeting in March 2023, the IJB approved the use of an element of contingency reserves to create a smoothing reserve to underwrite the delivery of the savings programme for 2023/24 of £0.594m and also to enhance the prescribing reserve by £1m to mitigate anticipated pressures related to increased price and volume demands during 2023/24. This provides a remaining balance on general reserves of £4.371m.
IJB’s are empowered under the Public Bodies (Joint Working) Scotland Act 2014 (section 13) to hold reserves and recommends the development of a reserves policy and reserves strategy. A Reserves policy was approved by the IJB on the 11 August 2016. This provides for a prudent reserve of 2% of net expenditure (less Set Aside) which equates to approximately £3.8m for the partnership. The level of general reserves is in line with this prudent level and provides the partnership with a contingency to manage any unexpected in year pressures moving into future years of financial uncertainty.
While contingency reserves have increased during 2022/23, there has been a net reduction in the level of earmarked reserves from £23.912m to £15.691m with the application of reserves in year to deliver on specific strategic priorities. During 2022/23, the HSCP used £12.891m of its earmarked reserves. In the main this related to the application of £2.930m towards Covid-19 expenditure incurred in year, the return of £7.034m to SG of the balance of Covid reserves as well as the use of reserves to support expenditure related to the delivery of PCIP, Action 15 and Oral Health priorities. There were some additions to earmarked reserves in year of £1.576m (related primarily to ADP, Adult Winter Support Funding and Community Link workers) along with the creation / enhancement of earmarked reserves as set out above totalling ££3.094m provides for an overall net reduction in earmarked reserves for the year of £8.221m. This will leave a balance on earmarked reserves of £15.691m.
The total level of partnership reserves is now £20.062m.
Financial Planning
In setting the budget for 2023/24, the partnership had a funding gap of £3.894m following an analysis of cost pressures set against the funding available to support health and social care expenditure in East Dunbartonshire, this is set out in the table below:
|
|
Delegated SW |
Delegated NHS |
Total HSCP |
|---|---|---|---|
|
Recurring Budget 2022/23 (excl. Set aside) |
69,918 |
92.118 |
162.036 |
|
SCS Budgets transferred to ED HSCP |
|
30.074 |
30.074 |
|
Set Aside |
|
38.382 |
38.382 |
|
Total recurring budget 2022/23 |
69.918 |
160.574 |
230,492 |
|
Financial Pressures 23/24 |
6.724 |
1,640 |
8,364 |
|
2023/24 Budget requirement |
76.642 |
162,214 |
238.856 |
|
2023/wr Financial settlement/Budget |
73.226 |
161.736 |
234,962 |
|
Financial challenge 23/34 |
3.416 |
0.478 |
3,894 |
|
Savings plan 23/24 |
(3.396) |
(0.498) |
(3,894) |
|
3,894 |
|
|
|
|
Residual Financial Gap 23/24 |
0.020 |
(0.020) |
(0.000) |
Savings plans of £0.3894m were identified to mitigate the financial pressures which delivered a balanced budget position moving into 2023/24. There are a number of significant financial risks to the HSCP moving into 2023/24 with uncertainty on the funding to support pay uplifts for Social Work staff, pressures in relation to prescribing expected to continue into the new financial year, pressures on contractual spend for Social Work care providers with funding only available to support the SLW element and risks to the delivery of the savings programme in full. This has necessitated the need to enhance prescribing reserves and to create a smoothing reserve to underwrite and phase in elements of the savings plan during 2023/24 with full delivery expected in future financial years.
The HSCP has a Medium Term Financial Strategy for the period 2023 – 2028 which outlines the financial outlook over the next 5 years and provides a framework which will support the HSCP to remain financially sustainable. It forms an integral part of the HSCP’s Strategic Plan, highlighting how the HSCP medium term financial planning principles will support the delivery of the HSCP’s strategic priorities.
There are a number of key opportunities and challenges for the HSCP at a national and local level. The most significant being the Review of Adult Social Care, elements of which have now been reflected in the new programme for government. This may see significant investment across a range of areas including the development of a National Care Services on an equal footing to the National Health Service, expansion of support for lower-level needs and preventive community support, increasing support to unpaid carers and sums paid for free personal care.
The HSCP has particular demographic challenges.
The longer term impacts of the pandemic (Covid-19) are yet to be fully assessed and the impact of this on the delivery of health and social care services.
The Financial Challenge
The Medium Term Financial Strategy (MTFS) for the HSCP provides a number of cost pressures with levels of funding not matching the full extent of these pressures requiring a landscape of identifying cost savings through a programme of transformation and service redesign. The MTFS was updated as part of the Budget Setting for 2023/24 in March 2023.
The main areas for consideration within the MTFS for the HSCP are:-
- The medium term financial outlook for the IJB provides a number of cost pressures with levels of funding not matching the full extent of these pressures requiring a landscape of identifying cost savings through a programme of transformation and service redesign.
- The IJB is planning for a range of scenarios ranging from best to poor outcomes in terms of assumptions around cost increases and future funding settlements. This will require the identification of £17.2m to £38.4m of savings (previously £11.5m to £21.8m) with the most likely scenario being a financial gap of £17.2m over the next five years.
- This will extend to £42.3m (previously £28.9m) over the next 10 years, however this becomes a more uncertain picture as the future environment within which IJBs operate can vary greatly over a longer period of time.
- Based on the projected income and expenditure figures the IJB will require to achieve savings between £4.1m and £4.5m (previously £0.5m and £3.0m) each year from 2023/24s onwards.
The aim of the medium term financial strategy is to set out how the HSCP would take action to address this financial challenge across the key areas detailed below:
Key areas identified to close the financial gap
Delivering services differently thorough transformation and service redesign
- Development of a programme for transformation and service redesign which focusses on identifying and implementing opportunities to redesign services using alternative models of care in line with ambitions of the HSCP Strategic Plan.
Efficiency Savings
- Implementing a range of initiatives which will ensure services are delivered in the most efficient manner.
Strategic Commissioning
- Ensuring that the services purchases from the external market reflect the needs of the local population, deliver good quality support and aline to the strategic priorities of the IJB.
Shifting the Balance of Care
- Progressing work around the un-scheduled care commissioning plan to address a shift in the balance of care away from hospital based services to services delivered within the community.
Prevention and Early Intervention
- Through the promotion of good health and wellbeing, self-management of long term conditions and intervening at an early stage to prevent escalation to more formal care settings.
Demand Management
- Implementing a programme focussed on managing demand and eligibility for services which enable demographic pressures to be delivered without increasing capacity. This is an area of focus through the Review of Adults Social Care.
Inspection and Regulation
Joint Inspections
On 26 September 2022 the Care Inspectorate wrote to the East Dunbartonshire Community Planning Partnership to advise that the Care Inspectorate, Education Scotland, Her Majesty’s Inspectorate of Constabulary in Scotland and Healthcare Improvement Scotland would undertake a joint inspection of services for children at risk of harm in East Dunbartonshire.
The remit of these joint inspections is to consider the effectiveness of services for children and young people up to the age of 18 at risk of harm. The inspections look at the differences Community Planning Partnerships are making to the lives of children and young people at risk of harm and their families.
The active phase of the inspection took place between October 2022 and February 2023 and the inspection report was published 18 April 2023. The report can be accessed on the Care Inspectorate’s publications web page [opens in a new window]
The inspection report highlights areas of good practice and areas for further development and concludes on an assessment grading for a single quality indicator 2.1, from the inspection framework, ‘impact on children and young people’. The inspection report has graded the services in East Dunbartonshire as ‘Good’. An evaluation of good is applied where performance shows important strengths which clearly outweigh any areas for improvement. The strengths will have been assessed as having a significant positive impact on children and young people’s experiences and outcomes.
The report highlighted the following strengths and areas of good practice:
- Many children and young people said that they got the right help to make and keep loving relationships with those they cared about. We saw how some were being supported to maintain relationships with brothers and sisters, as well as with parents.
- Support for children’s wellbeing, planning of care and provision of good nurturing relationships was rated as good or better in regulated care inspections.
- Almost all children and young people told us they felt safe where they lived all or most of the time. Asylum seeking young people felt well supported, safe and helped to maintain cultural links. Interpreters were provided for individual children or parents.
- Young people were being listened to about what mattered to them, felt involved and were aware of their rights. Many children and young people had the opportunity to develop consistent and enduring relationships with key staff.
- Children and young people had been directly engaged in service developments such as the House project. In other examples, including record keeping, they were influencing changes in practice.
- Staff we spoke with demonstrated a child-centred approach to providing services to improve the wellbeing of children and young people.
- Statutory and voluntary agencies were working well together to provide practical support for children, young people and their families. A range of services from pre-birth to teenage, provided early and effective intervention in response to emerging concerns.
- Children and young people had benefitted from their safety and wellbeing having been a key priority for leaders throughout the Covid-19 pandemic.
- The scrutiny partners concluded that they were confident that partners in East Dunbartonshire have the capacity to make changes to service delivery in the areas that require improvement. This was based on the following factors:
- Evidence of strong partnership working, and staff and leaders being committed to improving outcomes for children, young people and families.
- High levels of confidence from staff in their knowledge and abilities, supported by evidence from records reading.
- Similar levels of support from staff about their leaders’ ability to continue to drive change and make improvements.
- Well-developed management information and self-evaluation practice capable of identifying areas for improvement and further action.
- Collaborative inter-agency practice, including the role of the third sector, providing services to children at risk of harm and their families.
- Recent commitments to changes in practice, including the introduction of the Safe and Together model, and an emphasis on trauma informed practice.
- The partnership’s own self-evaluation had already identified many of the areas for improvement found by the inspection team, which showed that they knew themselves well and had a solid foundation to make improvements.
Scope for improvement was identified in awareness and consistent availability of advocacy services, further opportunities for the voices of children who were, or had been, at risk of harm to inform strategic planning, scope to improve the quality of chronologies, waiting times for access to specialist CAMHS services and scope to further develop analysis of impact and outcomes for children and their families.
An action plan has been developed in response and will be overseen by the Delivering for Children and Young People group on behalf of the Community Planning Partnership.
Service Inspections
Detail on Care Inspectorate evaluation grades relating to directly provided and arranged services is set out at Annex 2.
ANNEX 1: National Outcomes and Local Strategic Priorities & Enablers
The relationship between the National Health and Wellbeing Outcomes and the East Dunbartonshire HSCP Strategic Priorities and Enablers are set out in the chart below. The linkages shown are the ones that are most direct, but there may be other less direct associations:
East Dunbartonshire HSCP Strategic Priorities and Enablers
ANNEX 2: CARE INSPECTORATE EVALUATIONS – LOCAL SERVICES
The Care Inspectorate is the national regulator for care services in Scotland. The Care Inspectorate inspects services and evaluates the quality of care they deliver in pursuance of the National Care Standards. They support improvement in individual services and across the care sector nationally.
The Care Inspectorate will award grades for certain ‘quality themes’ that they have assessed. These ‘quality themes’ cover the main areas of a service’s work. How well the service performs in these areas will indicate how good the service is. One or more themes will be assessed, depending on the type of service and its performance history. A grade is given to each of the quality themes assessed using a six point grading scale, which works in this way:
| Grading scale | |
|---|---|
| Grade 6 - Excellent | Grade 3 - Adequent |
| Grade 5 - Very Good | Grade 2 - Weak |
| Grade 4 - Good | Grade 1 - Unsatisfactory |
The functions delegated to the HSCP Board include a statutory obligation to provide or arrange services to meet assessed care needs. The HSCP Board “directs” the Council to provide or arrange these services on its behalf. Some of these services are delivered directly by the Council and others are purchased from the third and independent sectors. It is important that the quality of the services we directly provide and those purchased are both of the highest quality. The Partnership works to improve its own services through direct management and operational oversight. Purchased services are subject to detailed specification and contract monitoring by the Partnership’s Commissioning Team. The grades of the services delivered by the Council and those purchased by the Partnership are set out below. The grades below are the most recent assessed by the Care Inspectorate for services based in East Dunbartonshire. Inspection reports can be found at on the Care Inspectorate website.
The Care Inspectorate now applies the National Care Standards. These have introduced new quality themes which will eventually apply to all registered services. The Care Inspectorate has begun applying these new quality themes.
The tables below have therefore separated out registered services by the framework of quality themes that were used as the basis of the inspections:
| Service | Wellbeing (previously Care & Support) |
Not Assessed Leadership (previously Management & Leadership) |
Staffing | Setting previously Environment) |
Care Planning (new Category) |
|---|---|---|---|---|---|
| HSCP / Council In-house Services | |||||
| Ferndale Care Home for Children & Young People | 5 | Not Assessed | Not Assessed | Not Assessed | 6 |
| Ferndale Outreach for Children & Young People | 5 | Not Assessed | Not Assessed | Not Assessed | 6 |
| John Street House | 5 | 4 | Not Assessed | Not Assessed | Not Assessed |
| Homecare Service Addendum: May 2023 service graded 5 in all categories (except Setting which was not inspected) | 5 | 4 | 5 | Not Assessed | 3 |
| Commissioned - Supported Accommodation | |||||
| Cornerstone Community Care | 5 | 5 | Not Assessed | Not Assessed | Not Assessed |
| Living Ambitions (Group registration covers Glasgow North & West Services) | 3 | 3 | Not Assessed | Not Assessed | Not Assessed |
| Independent Care Homes | |||||
| Abbotsford House | How good is our care and support during COVID-19 pandemic - 4 | ||||
| Antonine House | How good is our care and support during COVID-19 pandemic - 4 | ||||
| Ashfield | 5 | 4 | Not Assessed | Not Assessed | Not Assessed |
| Birdston Care Home | 4 | 4 | Not Assessed | Not Assessed | Not Assessed |
| Boclair Care Home | Registered August 2022, not been inspected | ||||
| Buchanan House | 3 | 3 | 3 | 4 | 4 |
| Buchanan Lodge | 4 | 4 | 4 | 4 | 4 |
| Buttercup House | 5 | Not Assessed | Not Assessed | Not Assessed | 4 |
| Campsie View | 3 | 4 | Not Assessed | Not Assessed | Not Assessed |
| Lillyburn | 5 | 5 | Not Assessed | Not Assessed | 5 |
| Mavisbank | Not Assessed | Not Assessed | 4 | Not Assessed | 4 |
| Milngavie Manor | 4 | 4 | Not Assessed | Not Assessed | Not Assessed |
| Mugdock | 5 | 5 | 5 | Not Assessed | Not Assessed |
| Springvale | 4 | 4 | 4 | 4 | 4 |
| Westerton | 4 | 4 | 4 | 4 | 4 |
| Whitefield Lodge | Not Assessed | Not Assessed | 3 | Not Assessed | Not Assessed |
| Commissioned – Care at Home Services | |||||
| Blue Bird Care | 4 | 4 | 4 | Not Assessed | Not Assessed |
| Cornerstone | 5 | 5 | Not Assessed | Not Assessed | Not Assessed |
| Hands-On Homecare | Not Assessed | 3 | 3 | Not Assessed | Not Assessed |
PREVIOUS INSPECTION MODEL:
|
Service |
Care and Support |
Environment |
Staffing |
Management and Leadership |
|---|---|---|---|---|
|
HSCP / Council In-house Services |
||||
|
Milan Day Service |
5 |
Not Assessed |
5 |
Not Assessed |
|
Allander Resource Centre |
5 |
Not Assessed |
5 |
Not Assessed |
|
Meiklehill & Pineview |
5 |
Not Assessed |
Not Assessed |
5 |
|
Fostering Service |
5 |
Not Assessed |
5 |
4 |
|
Adoption Service |
4 |
Not Assessed |
5 |
4 |
|
Community Support Team for Children and Families |
5 |
Not Assessed |
Not Assessed |
6 |
|
Commissioned - Supported Accommodation |
||||
|
Key Housing Association – Key Community Supports – Clyde Coast (Group registration covers Milngavie, Kirkintilloch, Clydebank, Alexandria & Dalmuir) |
5 |
Not Assessed |
Not Assessed |
5 |
|
Orems Care Services |
4 |
Not Assessed |
4 |
Not Assessed |
|
Quarriers (Phase 3) |
4 |
Not Assessed |
4 |
Not Assessed |
|
Quarriers (Phase 2) |
4 |
Not Assessed |
4 |
4 |
|
Quarriers (Phase 1) |
5 |
Not Assessed |
Not Assessed |
4 |
|
Real Life Options East Dunbartonshire Service |
5 |
Not Assessed |
5 |
Not Assessed |
|
The Richmond Fellowship East & West Dunbartonshire Support Living Services |
5 |
Not Assessed |
Not Assessed |
5 |
|
Commissioned – Care at Home Services |
||||
|
Delight Supported Living |
5 |
Not Assessed |
5 |
Not Assessed |
|
Extended Personal Care |
4 |
Not Assessed |
4 |
Not Assessed |
|
Home Instead |
5 |
Not Assessed |
Not Assessed |
4 |
|
The Richmond Fellowship – East and West Dunbartonshire |
5 |
Not Assessed |
Not Assessed |
5 |
ANNEX 3: COMPARATIVE INCOME & EXPENDITURE 2015/16 – 2022/23
| Objective Analysis | 2022/23 | 2021/22 | 2020/21 | 2019/20 | 2018/19 | 2017/18 |
|---|---|---|---|---|---|---|
| Strategic / resources | 3,743 | 3,044 | 2,568 | 3,042 | 3,205 | 3,648 |
| Addictions | 1,692 | 1,351 | 1,369 | 1,285 | 1,360 | 1,253 |
| Older people | 47,551 | 42,664 | 38,644 | 39,410 | 36,916 | 34,531 |
| Learning disability | 23,380 | 20,479 | 19,333 | 19,580 | 18,559 | 18,068 |
| Physical disability | 5,093 | 5,005 | 4,880 | 4,067 | 4,042 | 4,003 |
| Mental health | 6,057 | 5,520 | 5,378 | 5,155 | 5,129 | 5,349 |
| Adult services | ||||||
| Children & families | 14,930 | 14,795 | 14,262 | 14,277 | 13,514 | 13,056 |
| Criminal justice | 455 | 346 | 162 | 211 | 258 | 226 |
| Other - non sw | 984 | 810 | 741 | 817 | 946 | 1,198 |
| Community health services | ||||||
| Oral health | 12,738 | 10,786 | 9,820 | 9,835 | 9,899 | 9,632 |
| Family health services | 33,218 | 31,314 | 29,822 | 27,678 | 25,848 | 24,724 |
| Prescribing | 22,027 | 19,936 | 19,178 | 19,484 | 19,072 | 19,473 |
| Covid-19 | 2,930 | 6,245 | 7,215 | |||
| Operational costs | 304 | 289 | 282 | 270 | 246 | 234 |
| Cost of Services Managed By East Dunbartonshire HSCP | 175,101 | 162,584 | 145,111 | 145,111 | 138,995 | 135,394 |
| Set Aside for Delegated Services provided to Acute Services | 40,306 | 35,982 | 36,975 | 32,247 | 27,471 | 17,381 |
| Total Cost of Services to East Dunbartonshire HSCP | 215,407 | 198,566 | 190,629 | 177,358 | 166,466 | 152,775 |
| NHS Greater Glasgow & Clyde | (137,042) | (149,959) | (144,950) | (120,508) | (111,583) | (99,721) |
| East Dunbartonshire Council | (71,437) | (62,753) | (57,719) | (55,760) | (52,690) | (51,910) |
| Taxation & Non Specific grant Income | (208,479) | (212,712) | (202,669) | (176,268) | (164,273) | (151,631) |
| (Surplus) or deficit on Provision of Services | 6,928 | (14,146) | (12,040) | 1,090 | 2,193 | 1,144 |
| Movement in Reserves | 6,928 | (14,146) | (12,040) | 1,090 | 2,193 | 1,144 |
| General Reserves | 2022/23 | 2021/22 | 2020/21 | 2019/20 | 2018/19 | 2017/18 |
|---|---|---|---|---|---|---|
| Movement in General Reserves only | (1,293) | (1.143) | (1,935) | 41 | 916 | 1,703 |
| Balance on Reserves | (4,371) | (3,078) | (1,935) | 0 | (41) | (957) |
ANNEX 4: ACHIEVEMENT OF BEST VALUE
| Best Value Audit June 2023 – HSCP Evaluation | ||
|---|---|---|
| 1 | Who do you consider to be accountable for securing Best Value in the IJB | Integration Joint Board Integration Joint Board Performance, Audit & Risk Committee HSCP Chief Officer HSCP Chief Finance & Resources Officer Senior Management Team HSCP Leadership Group and Forum Parent Organisations around support services, assets and all staff who are involved in commissioning and procurement. All staff involved in the prescription of packages of care, drugs and drugs (acting in line with agreed policies etc.) |
| 2 | How do you receive assurance that the services supporting the delivery of strategic plans are securing Best Value |
Performance management reporting on a quarterly basis to IJB. |
| 3 | Do you consider there to be a sufficient buy-in to the IJB’s longer term vision from partner officers and members | Yes, the IJB has approved a Medium Term Financial Strategy 2022 - 2027 setting out the financial outlook, challenges and strategy for managing the medium term financial landscape. This is reviewed annually. This is aligned to its Strategic Plan which clearly sets out the direction of travel with work underway to develop and engage on the next iteration of the Strategic Plan. The IJB has good joint working arrangements in place and has benefited from ongoing support, within the resources available, in support of service redesign, from members and officers within our partner organisations over the past 12 months in order to deliver the IJBs longer term vision. Engagement with partner agency finance leads to focus on budget performance, financial planning in support of delivery of strategic priorities. Bi Annual OPR meetings with partner agency Chief Executives to focus on performance and good practice and any support required to progress initiatives. (frequency impacted through Covid-19 response / recovery and to be re-established) |
| 4 |
Monthly budget reports and scrutiny at service level and regular budget meetings with managers across the HSCP. |
|
| 5 | Do you consider there to be a culture of continuous improvement? |
The HSCP has an overarching Quality Management Framework that establishes a cultural and operational commitment to continuous improvement. This is being implemented across the HSCP with a Governance post now in place to provide effective oversight and monitoring of consistent quality aspects set out within the framework. Focus on self-evaluation work as a means for identifying improvement and preparation for strategic inspections.
|
| 6 | Have there been any service reviews undertaken since establishment – have improvements in services and/or reductions in pressures as a result of joint working? |
A robust process for progressing service reviews is in place with support from the Council’s transformation team where appropriate. A number of reviews have been undertaken including:
The HSCP is also participating in a number of reviews in collaboration with NHS GGC such as
There are a number of work streams to be progressed through the HSCP Annual Delivery Plans which sets out the transformation activity for the year and the strategic areas of work the HSCP will be progressing during 23/24. |
| 7 | Have identified improvement actions been prioritised in terms of those likely to have the greatest impact. | The oversight for any improvement activity identified through service review, inspection reports, incident reporting or complaints learning is through the Clinical and Care Governance Group. This is reported through the SMT, the Performance, Audit & Risk Committee and the IJB to ensure priority is afforded to progress areas of high risk with scope for most improvement. The Annual Delivery Board has a role to consider and oversee service redesign which will deliver service improvement including robust business cases and progress reporting to ensure effective delivery in line with strategic planning priorities and quality care governance and professional standards. |
| 8 | What steps are taken to ensure that quality of care and service provided is not compromised as a result of cost saving measures. |
All savings proposals are subject to a full assessment which includes:
Where possible, the HSCP look to take evidence based approaches or tests of change to ensure anticipated benefits are realised and there is no compromise to care. |
| 9 | Is performance information reported to the board of sufficient detail to enable value of money to be assessed | Regular budget and performance monitoring reports to the IJB give oversight of performance against agreed targets with narrative covering rationale, situational analysis and improvement actions for areas where performance is off target. These reports are presented quarterly as well as the detailed Annual Performance Report. Financial performance reported every cycle to IJB. Plans to revise format of performance report to include finance narrative to provide linkages of impact of performance on the partnership financial position. The Annual Service Delivery Plan aligns key priorities for service redesign and transformation to the delivery of efficiency savings which are regularly reported through the Financial monitoring reports to the IJB and regular scrutiny of the transformation plan through the Performance, Audit and risk committee. |
| 10 | How does the IJB ensure that management of resources (finances, workforce etc.) is effective and sustainable | Workforce and Organisational Development plan linked to strategic plan. Oversight through Staff Partnership Forum and reporting through the IJB. Service review process involves staff partnership representation for consideration of workforce issues. Regular budget and performance monitoring reports to the IJB give oversight of this performance. Financial planning updates to the IJB on budget setting for the partnership highlighting areas for service redesign, impact and key risks. Regular review and update on reserves positions as a means of providing contingency to manage any in year unplanned events. All IJB reports contain a section outlining the financial implications of each paper for consideration. |
ANNEX 5: NOTES ON PERFORMANCE DATA METHODOLOGY
The Scottish Government operate two sets of indicators to monitor performance across core integration functions. These relate principally to adult health and social care functions:
- Core National Integration Indicators
- Ministerial Strategic Group (MSG Indicators
Notes on Core National Integration Indicators
Indicators 1-9 are reported by a national biennial Health and Social Care Experience Survey that reports every two year. The most recent data for this is 2021/22. East Dunbartonshire had a response rate of 30%, which equates to 2,400 returns, compared to a Scotland response rate of 24%, which equates to 130,000 returns. It is important to note the limitations of the survey due to small numbers, which introduces a margin of error at a local level. Comparison of “performance” using this data should therefore be seen as an approximation.
Please note figures for the years from 2019/20 for indicators 2, 3, 4, 5, 7 and 9 are not directly comparable to figures in previous years due to changes in methodology.
More information on the survey and changes in the methodology are available by clicking here:selecting this link to the Scottish Government Health Care Experience Survey. [opens in a new window]
Indicators 12, 13, 14, 15, 16 and 20
The primary sources of the remaining data for these indicators are Scottish Morbidity Records (SMRs) which are nationally collected discharge-based hospital records. Annual figures for these indicators are presented by financial year until the most recent reporting year. In accordance with recommendations made by Public Health Scotland (PHS) and communicated to all Health and Social Care Partnerships, the most recent reporting period available is calendar year 2022; this ensures that these indicators are based on the most complete and robust data currently available and acts as a suitable proxy, for comparison purposes.
Indicator 20 presents the cost of emergency admissions as a proportion of total health and social care expenditure. Information for this indicator was previously published up to calendar year 2020 but is now presented to financial year 2019/20 only. PHS have recommended that Integration Authorities do not report information for this indicator beyond 2019/20 within their Annual Performance Reports.
More detail is provided in the Background and Glossary document is available by selecting the
Public Health Scotland Core Suite of Integration Indicators. [opens in a new window]
Trends and National Rankings
The tables and charts aim to illustrate whether the objective is to increase or decrease the performance value, they show our performance in the reporting year, our performance trend compared to the previous year, our performance trend over the period since the integration of health and social care, our comparative performance over the same period and our “ranking” against the 31 other HSCPs in Scotland (Clackmannanshire & Stirling are a joint HSCP). Regardless of whether the objective is to increase or decrease the performance value, in ranking terms, 1 is always the best performing HSCP and 31 is the least well performing HSCP. With a number of indicators though, HSCPs perform at very similar levels, so trend lines can be very close together and national rankings should be viewed cautiously in situations where very tight clustering of performance levels exist. For these reasons, the tables and charts should be viewed in a balanced way that takes into account these factors.
Ministerial Strategic Group (MSG) – Performance Indicators
This measures provides data and performance status of the HSCP’s performance against the Scottish Government’s Ministerial Strategic Group’s indicators. Performance using a “Red-Amber-Green” (RAG) rating is based upon comparison with the previous year. A chart showing comparative performance against the Scottish average is also provided.
For indicators 1 and 2 annual data are presented by financial year until the latest reporting year. As April 2022 to March 2023 data is not fully complete for all NHS Boards, calendar year figures are shown for 2022 as a proxy for financial year data.
Impact of Coronavirus (COVID-19)
Depending on the stage of the pandemic, COVID-19 may have an impact on trends observed for certain indicators across certain periods, particularly those based on hospital activity information (indicators 12, 13, 14, 15, and 16 and MSG indicators). The “bounce-back” from the Covid-19 related downturn in hospital activity also results in exaggerated single year trends for these indicators.